A. Radiation therapy
B. Total parenteral nutrition
C. Hepatorenal syndrome
D. Iodine deposition
For patients in questions 3 to 7, select the most likely diagnosis (A to F) for the hepatic masses. Each option may be used once, more than once, or not at all.
A. Cavernous hemangioma
B. Hepatocellular adenoma
C. Focal nodular hyperplasia
D. Hepatocellular carcinoma
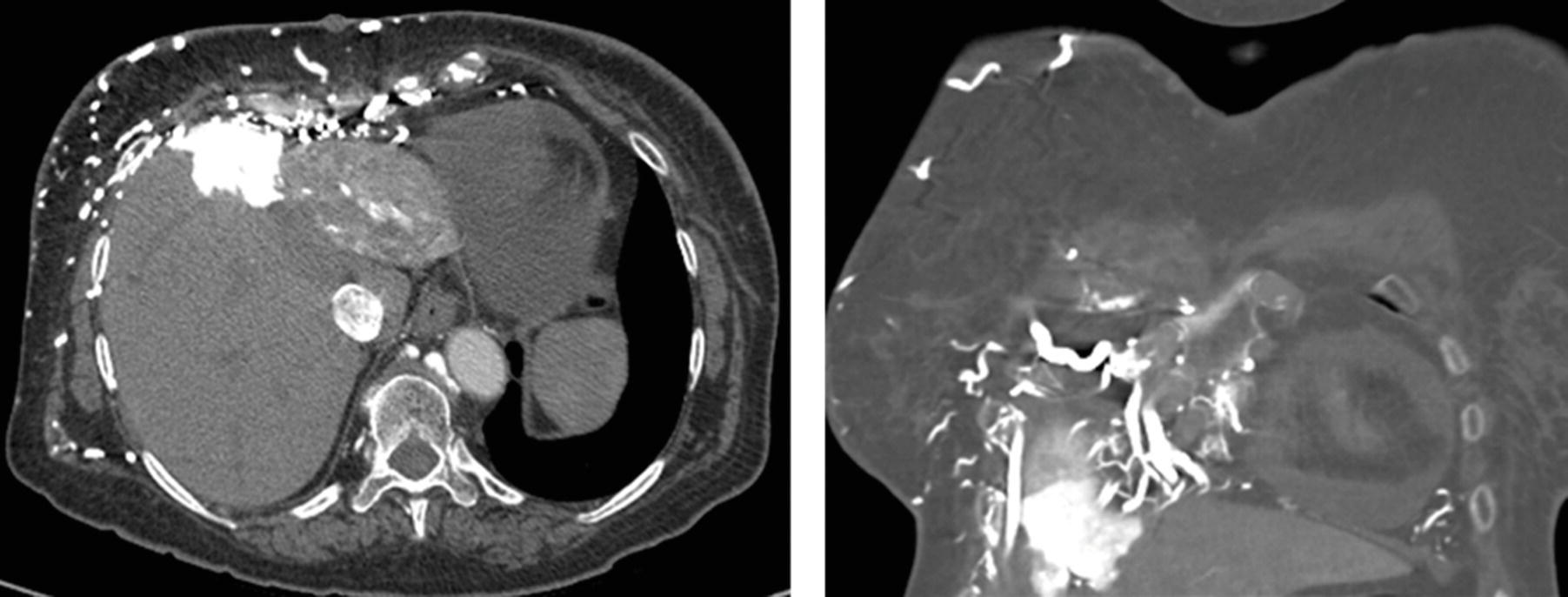
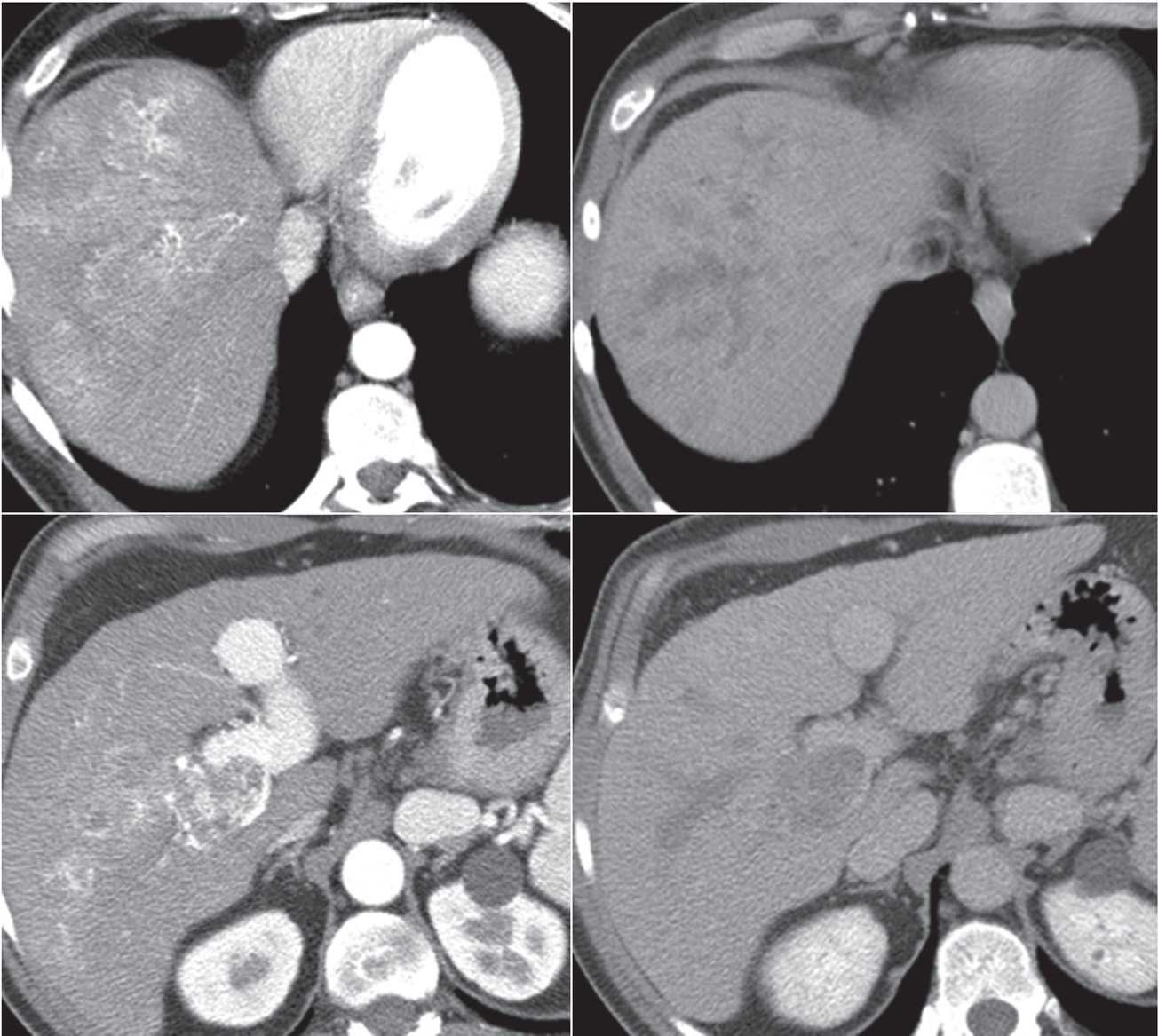
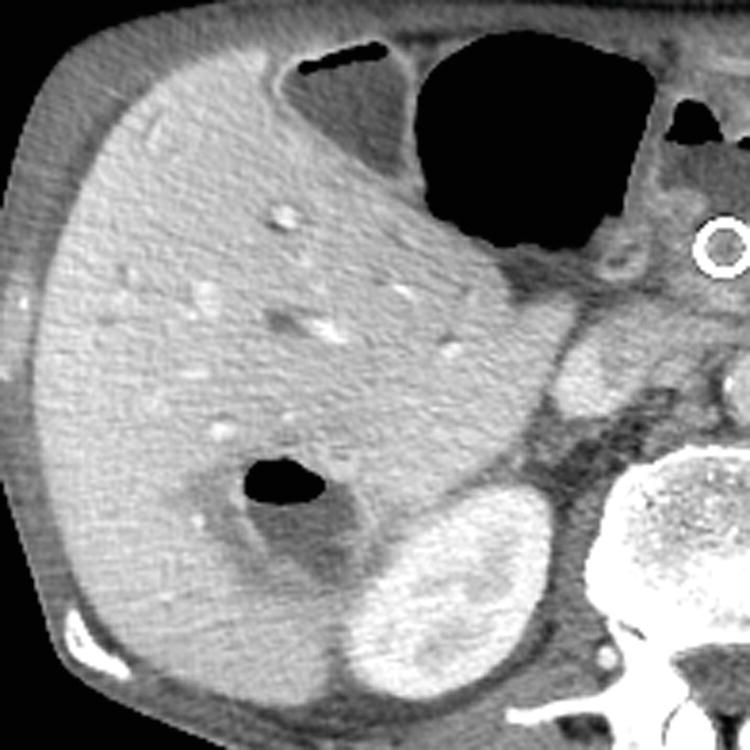
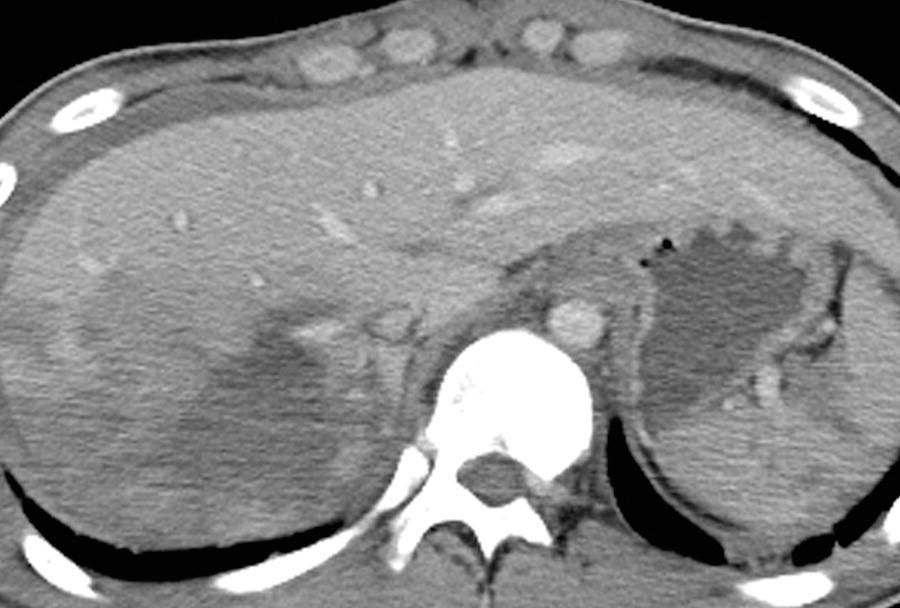
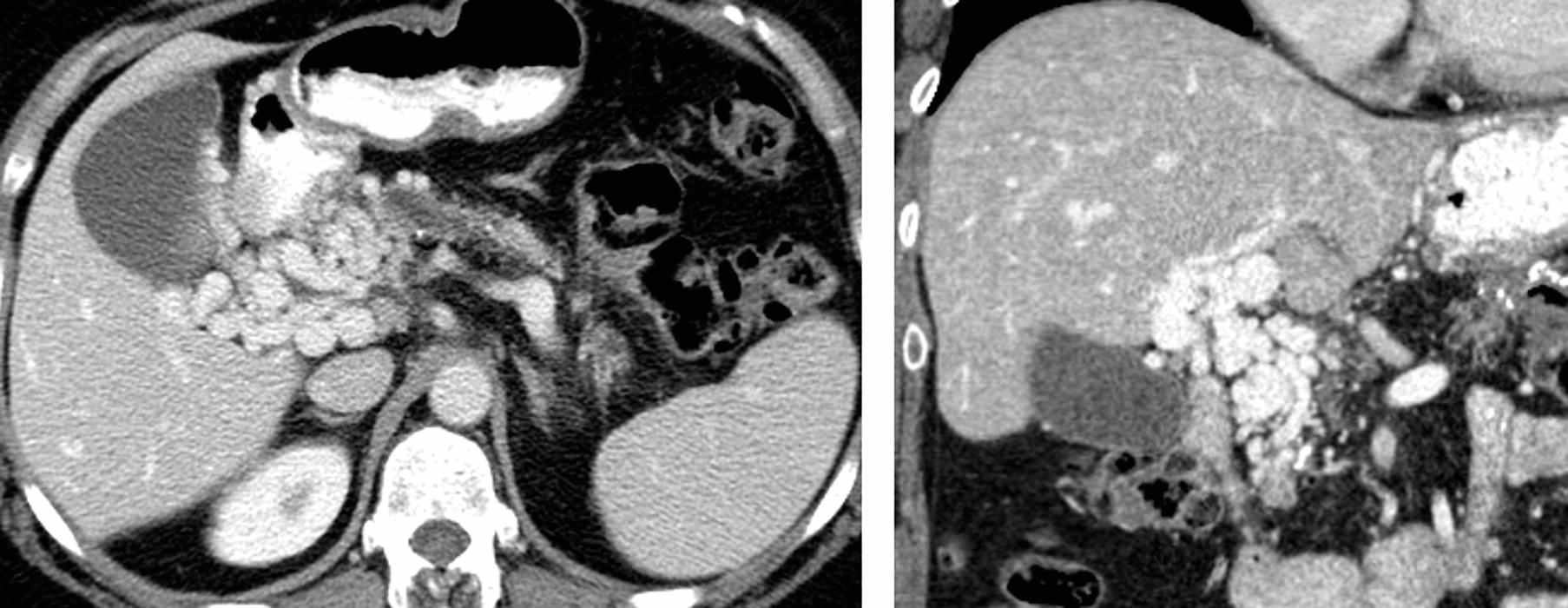
E. Cholangiocarcinoma
F. Abscess
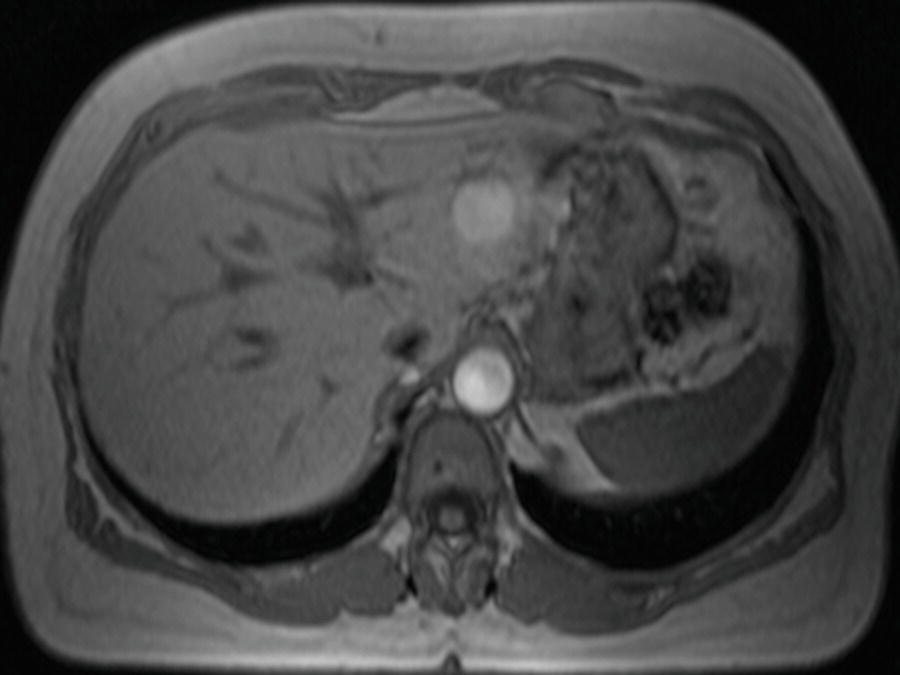
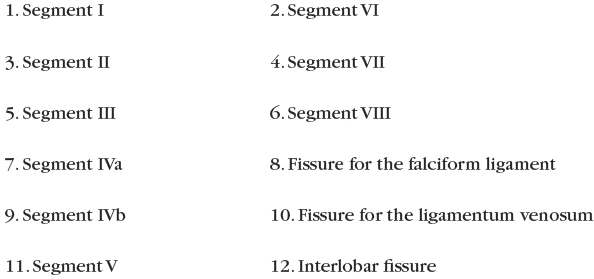
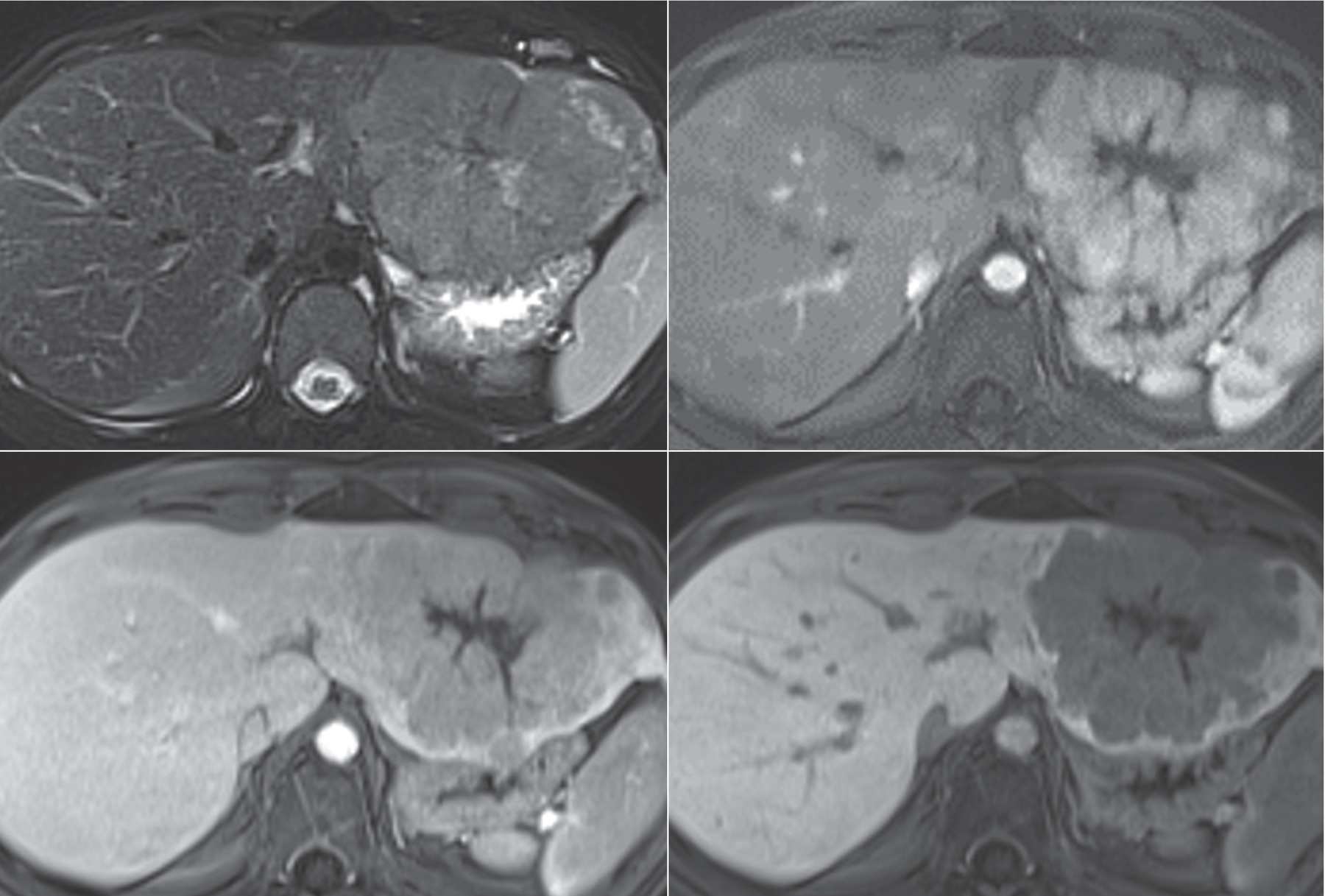
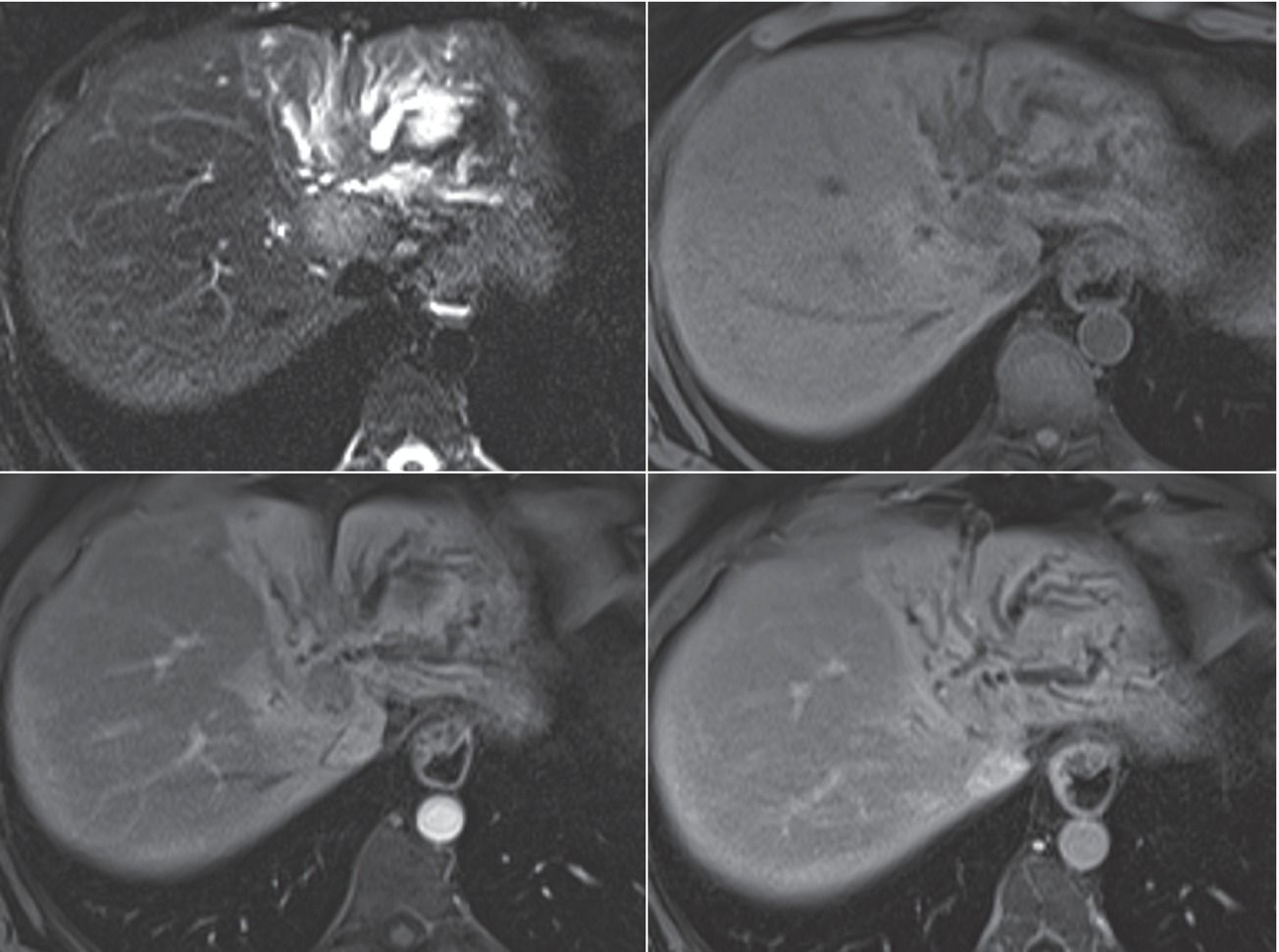
3 A 63-year-old woman with right upper quadrant pain and a liver finding noted on ultrasound. Images are from an MRI using conventional extracellular gadolinium contrast.
FS T2W, arterial phase T1W+gad, and delayed phase T1W+gad.
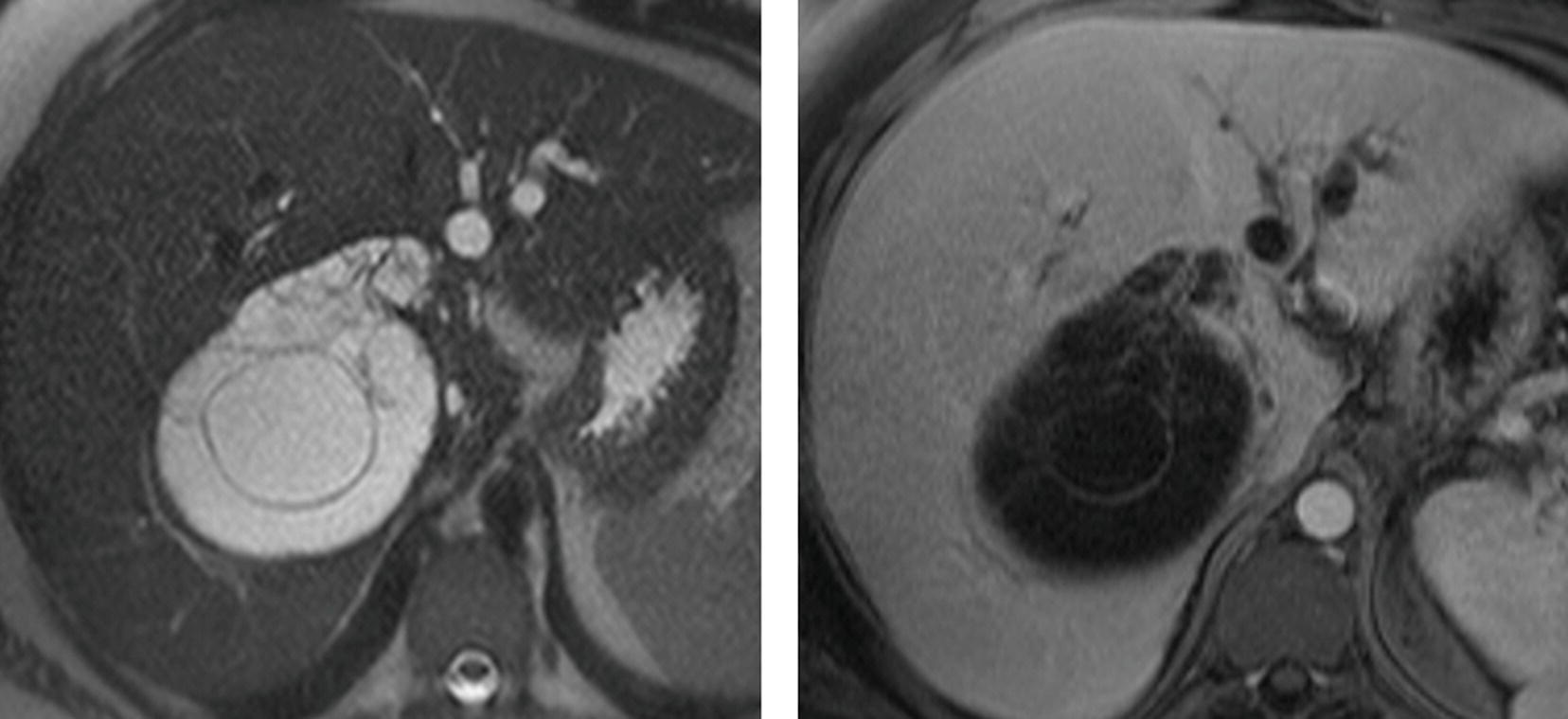
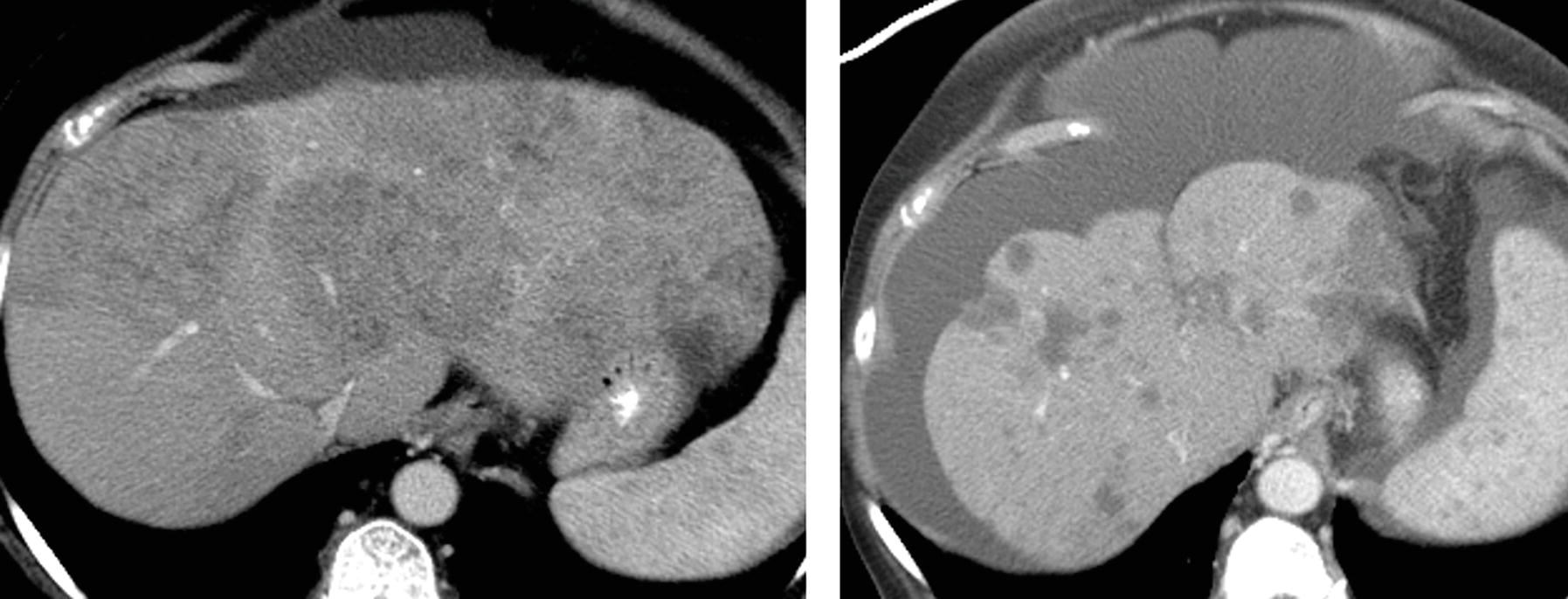
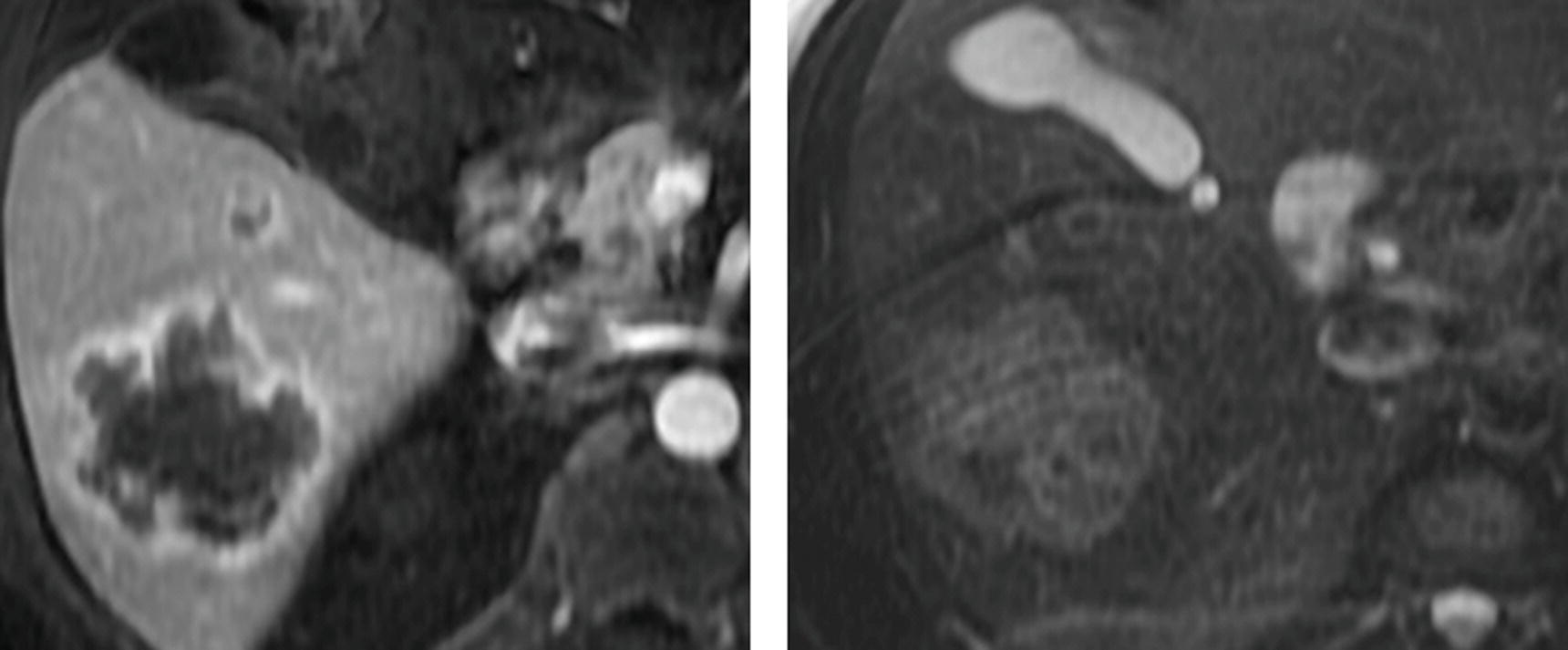
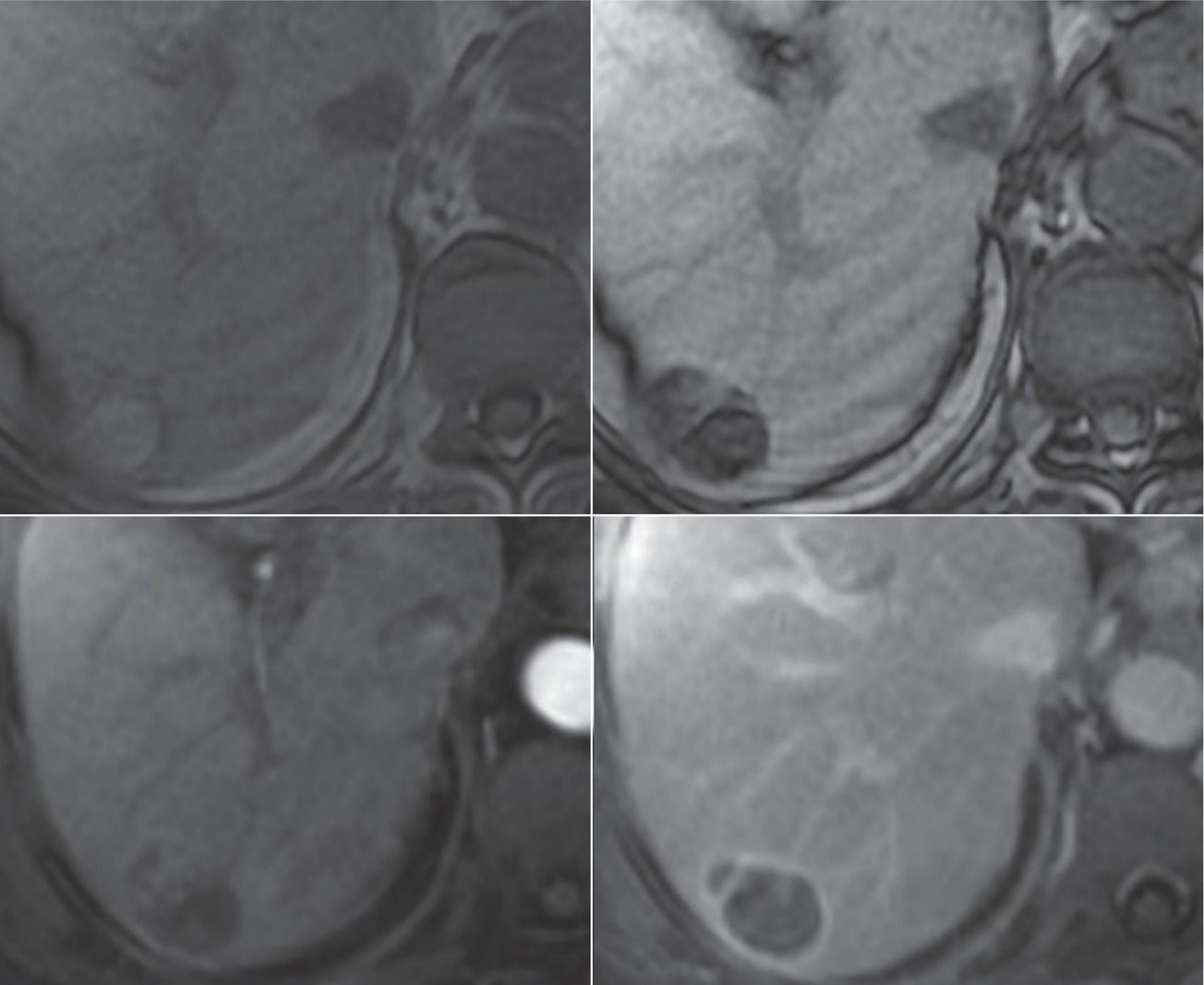
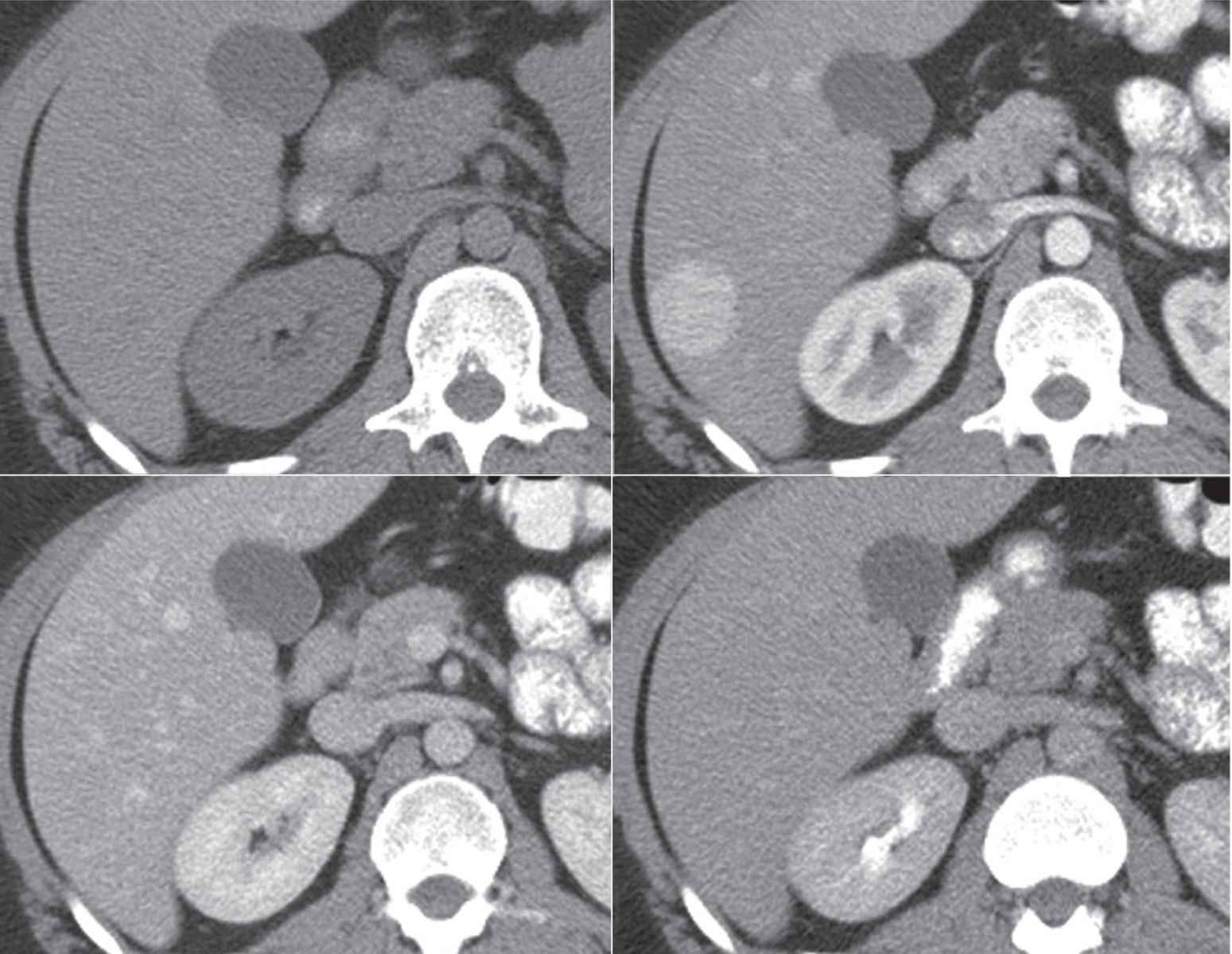
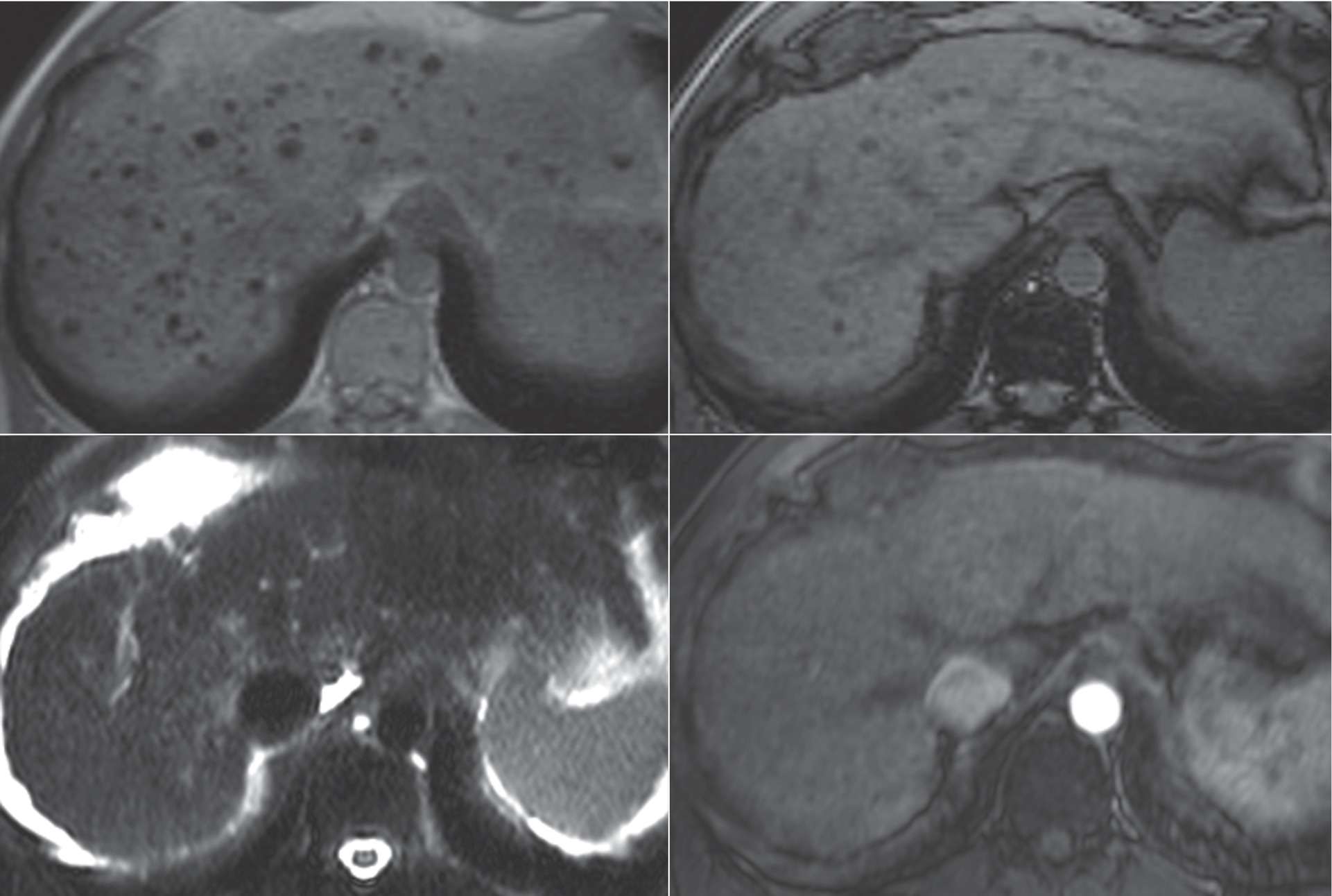
4 A 47-year-old woman with cirrhosis secondary to hepatitis C. Images from an MRI performed with conventional extracellular gadolinium contrast are shown.
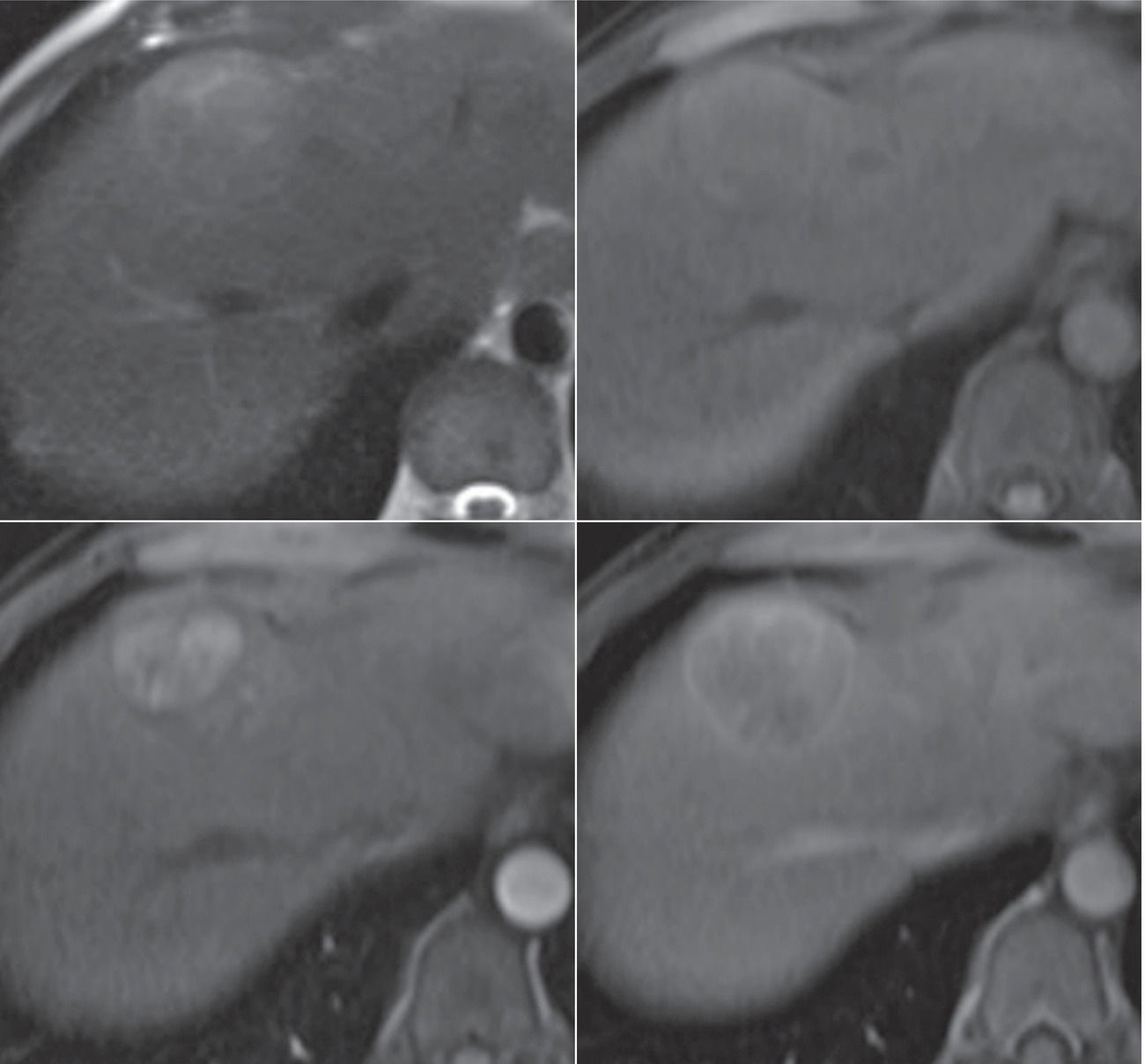
Top row: T2W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
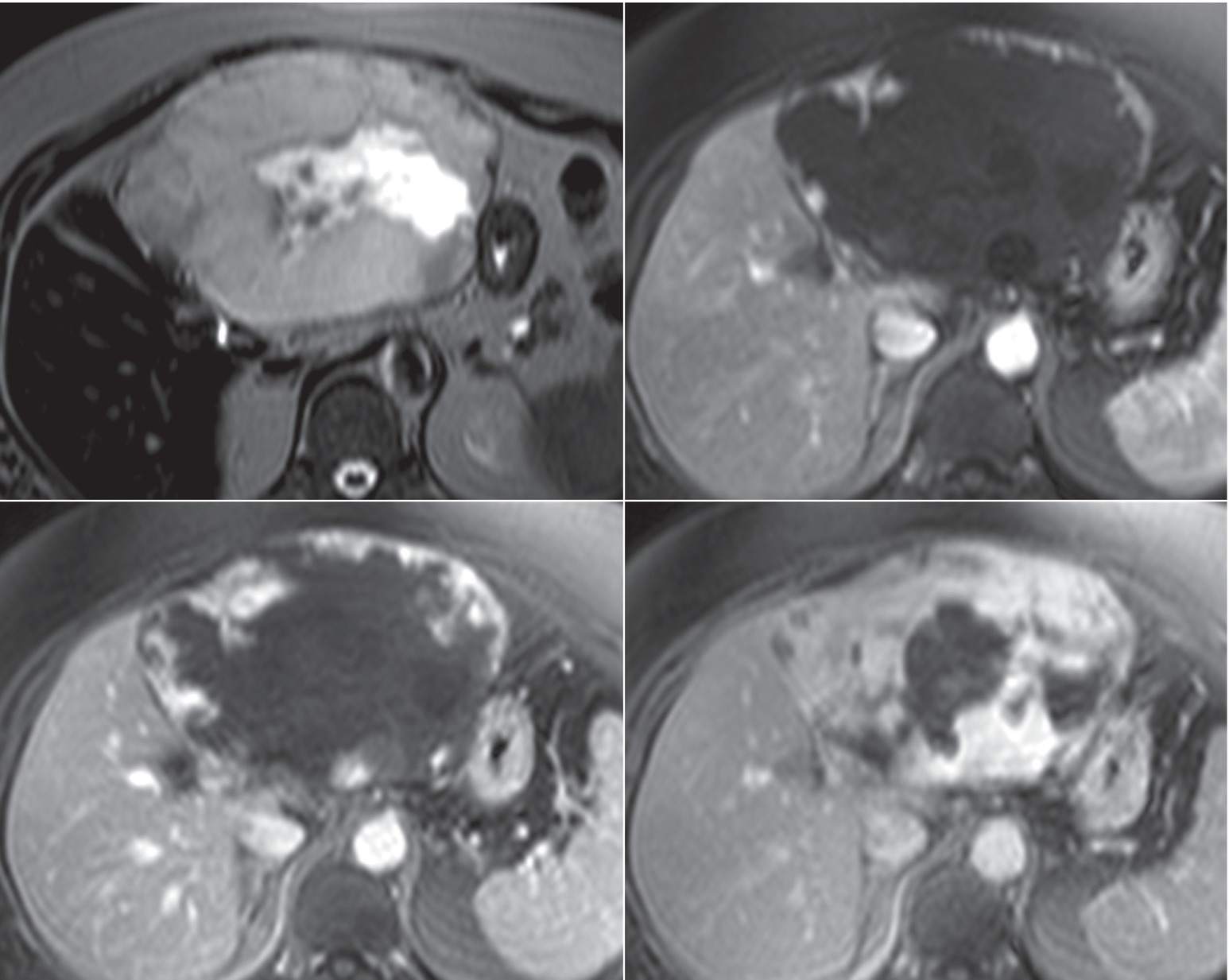
5 A 46-year-old woman with painless jaundice. Images from an MRI performed with conventional extracellular gadolinium contrast are shown.
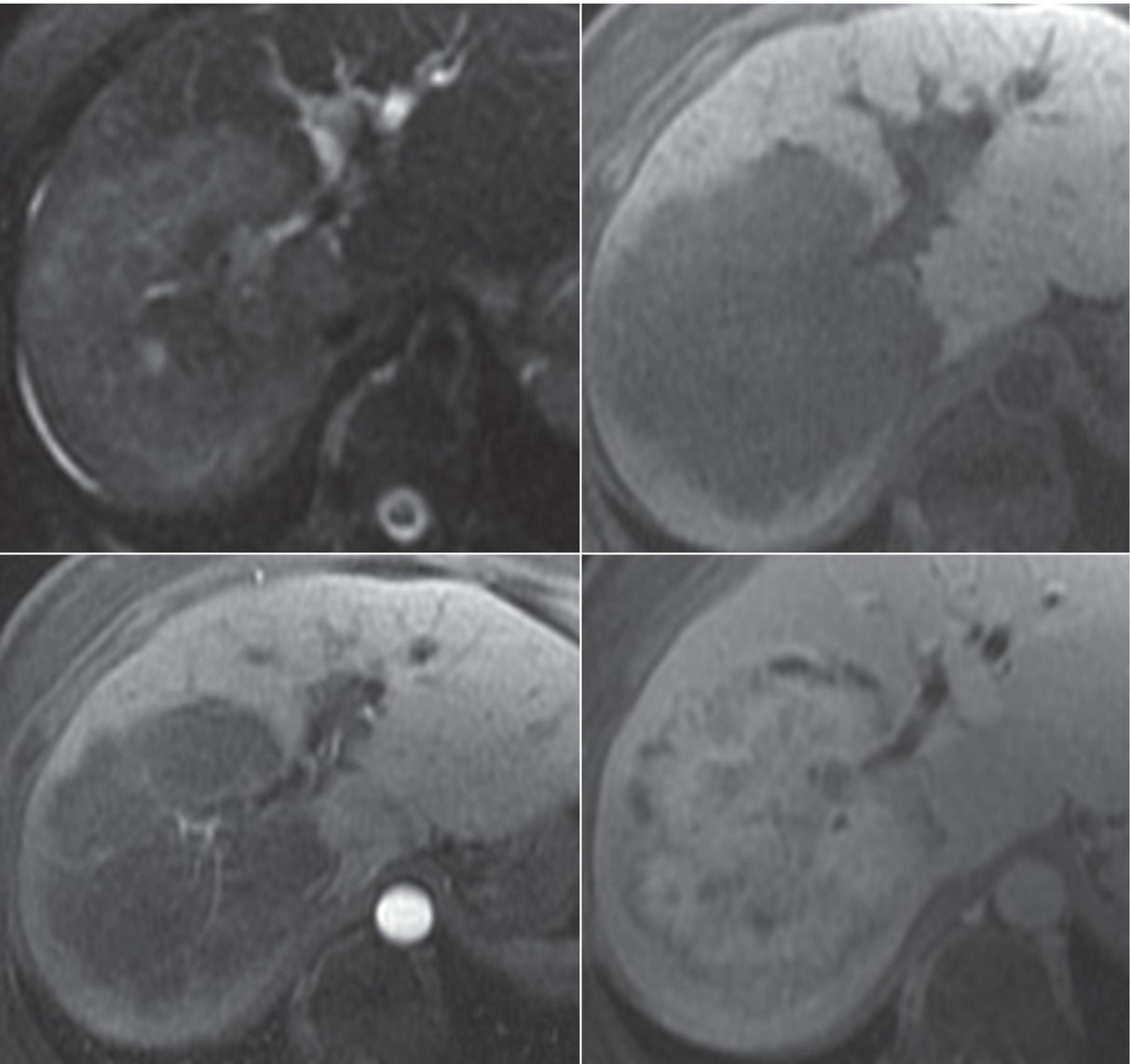
Top row: T2W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
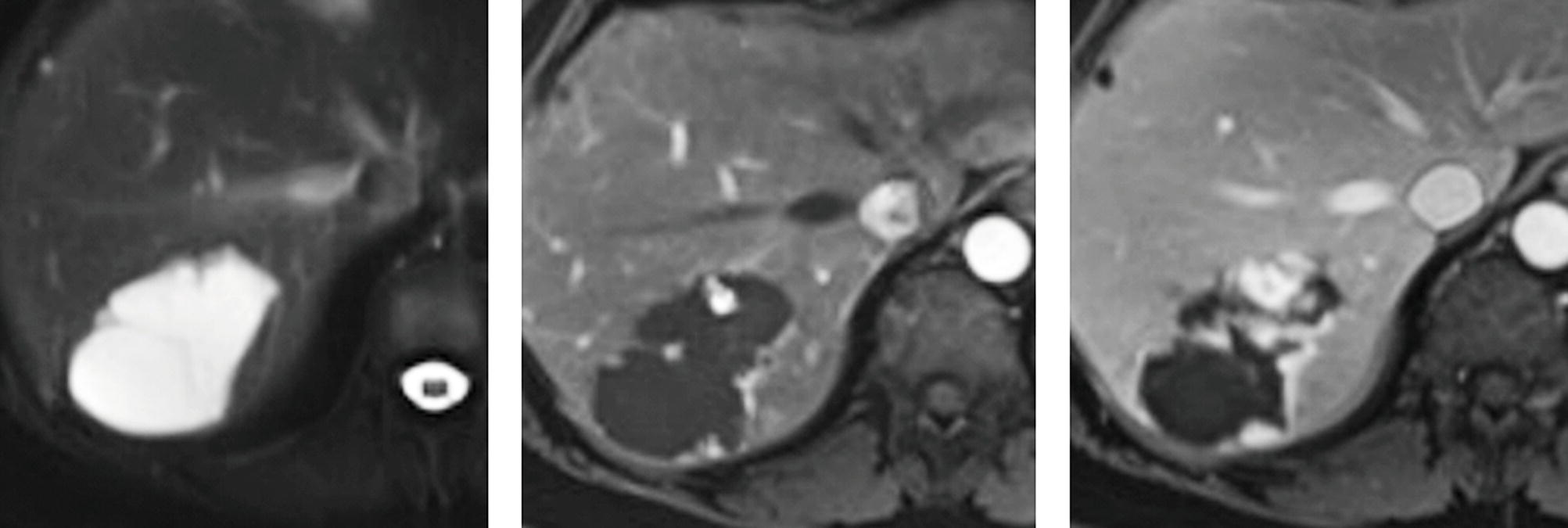
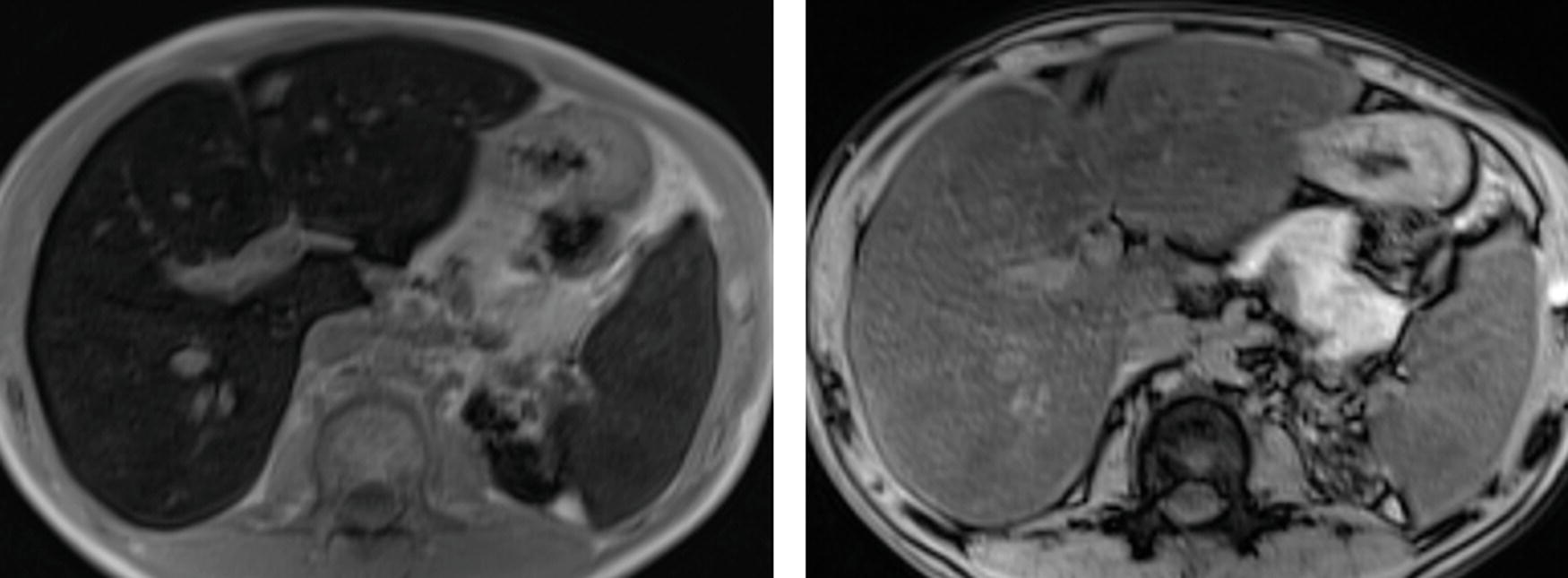
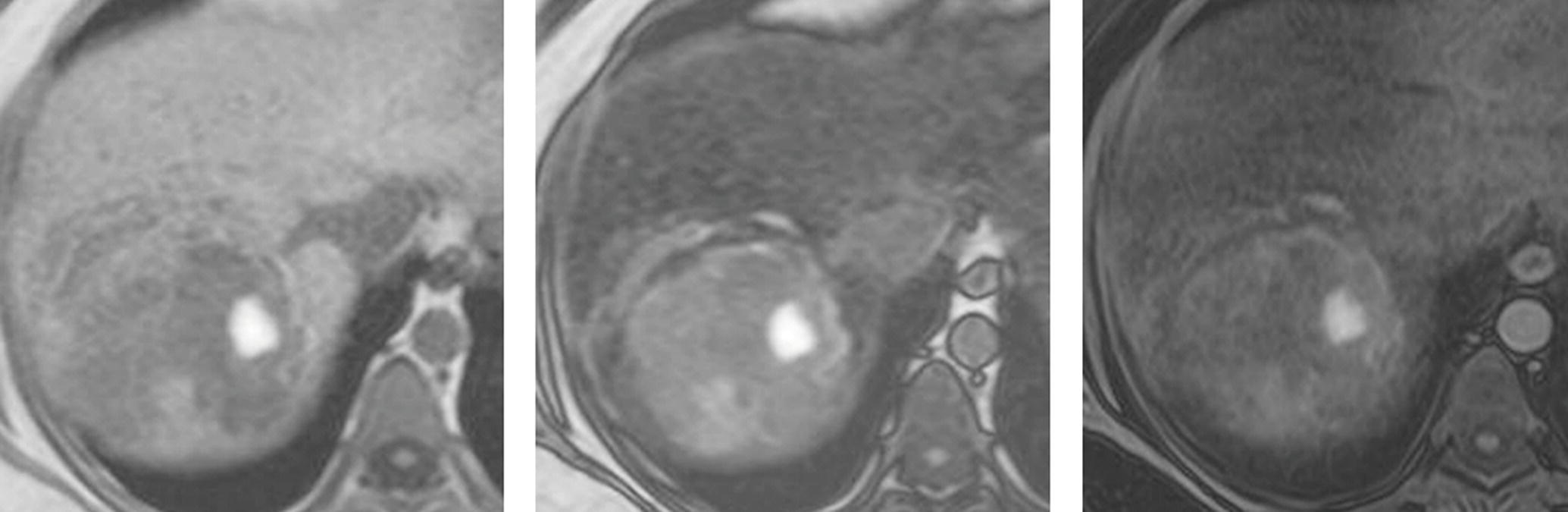
6 A 21-year-old woman found to have a liver lesion on ultrasound. Images from an MRI using hepatobiliary gadolinium contrast agent gadoxetate disodium (Eovist—Bayer HealthCare) are shown.
T2W, arterial phase FS T1W+hepatobiliary gad, and 20-minute FS T1W+hepatobiliary gad.
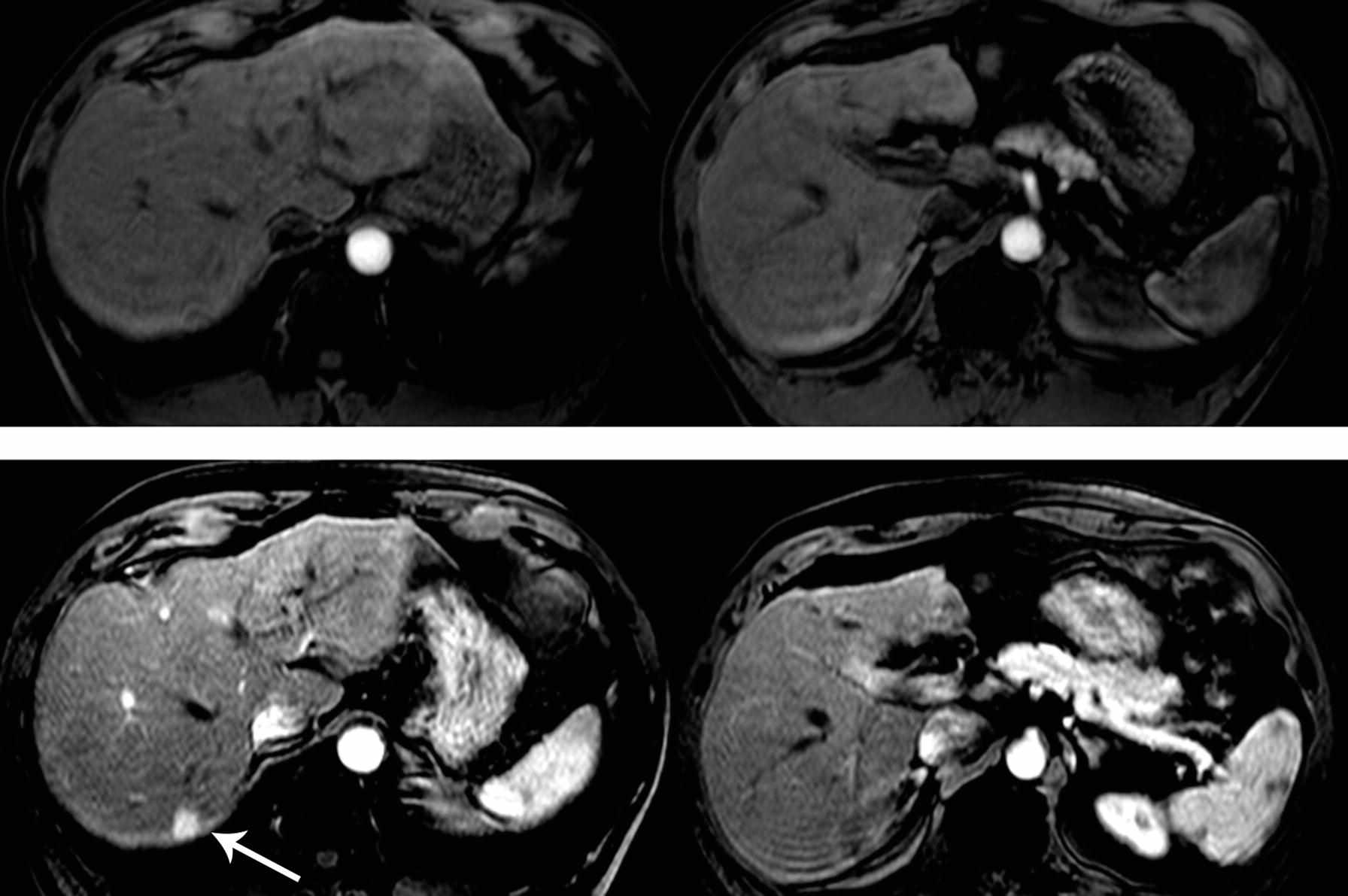
7 A 51-year-old man with hepatitis B and cirrhosis. Images from an MRI performed with hepatobiliary contrast agent are shown.
FS T2W, arterial phase FS T1W+hepatobiliary gad, and a 20-minute FS T1W+hepatobiliary gad.
8 Which of the following would be considered an ancillary feature favoring hepatocellular carcinoma rather than a major feature according to the Liver Imaging Reporting and Data System (LI-RADS)?
A. Washout appearance
B. Capsule appearance
C. Arterial enhancement
D. Hepatobiliary phase hypointensity
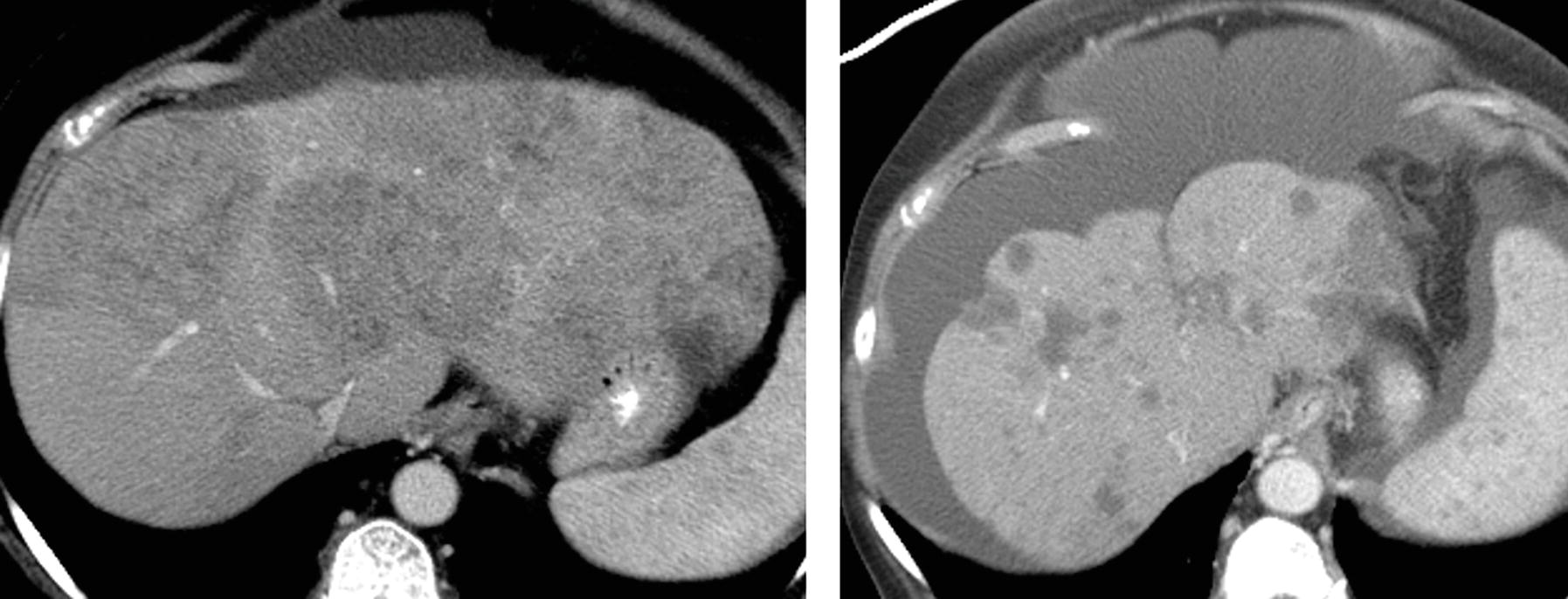
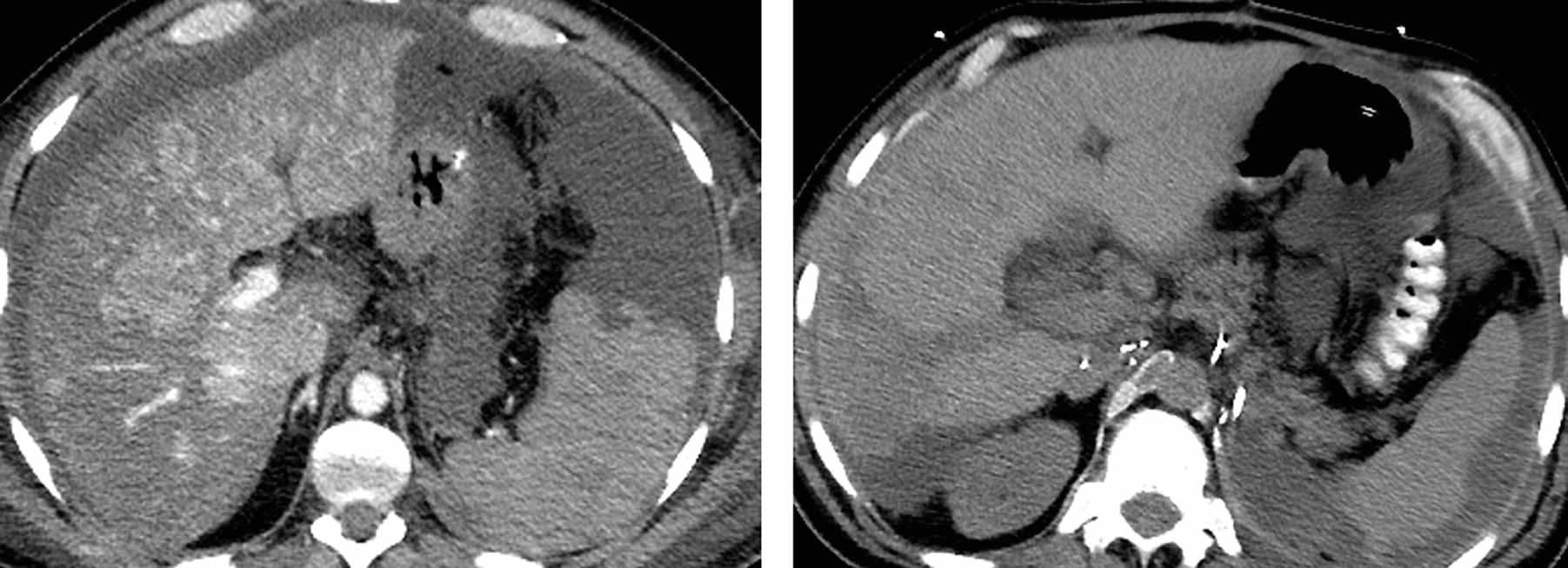
9 Images from a CT on a 55-year-old man with hepatitis C and cirrhosis are shown. Arterial phase images are shown on the left, and delayed images are shown on the right. Which LI-RADS category best fits the findings?
A. LR-2 probably benign
B. LR-3 intermediate probability for hepatocellular carcinoma
C. LR-4 probably hepatocellular carcinoma
D. LR-5 definitely hepatocellular carcinoma
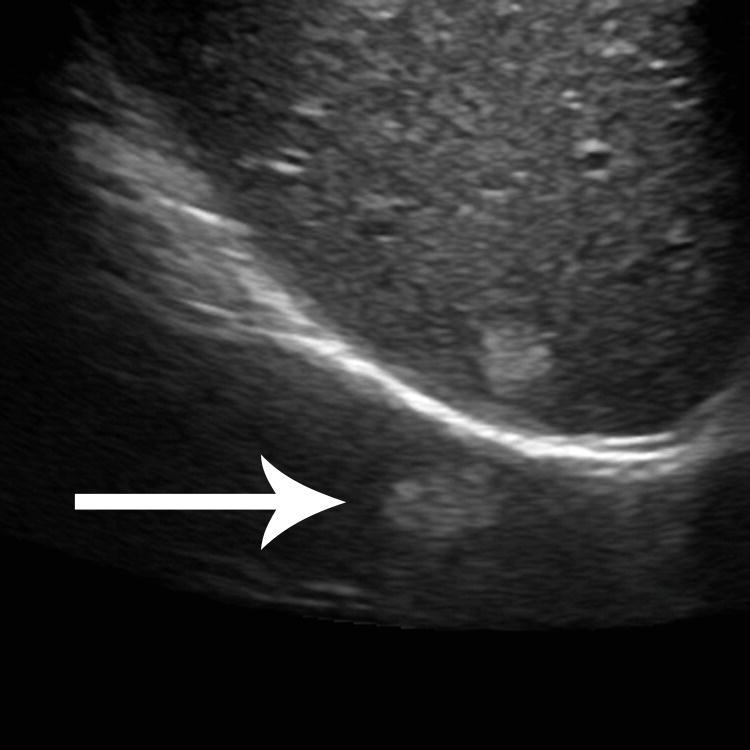
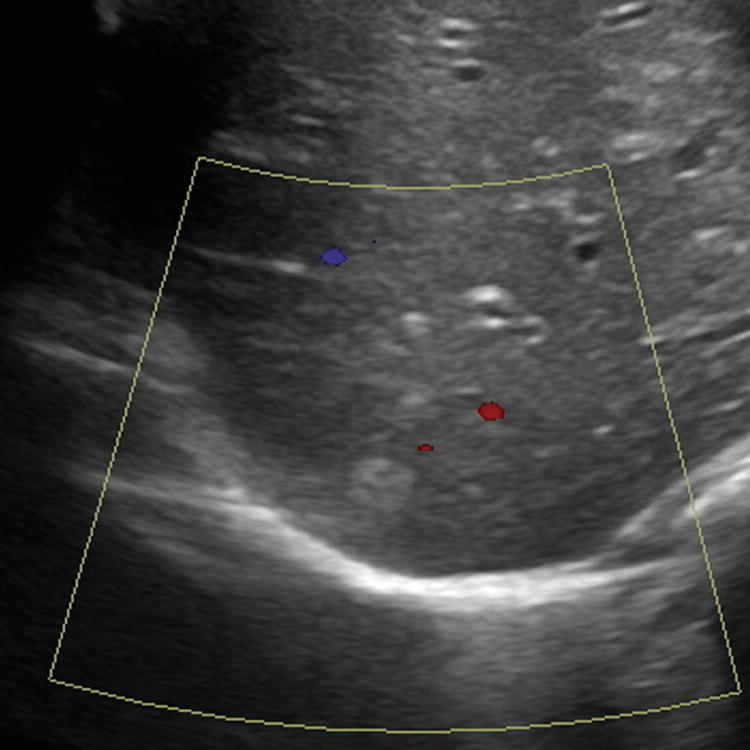
10a A 24-year-old man with no history of liver disease presents with epigastric pain and vomiting. A transverse image from an abdominal ultrasound is shown. What is the most likely diagnosis?
A. Hemangioma
B. Hepatocellular carcinoma
C. Angiomyolipoma
D. Metastasis
A. Lung nodule
B. Mirror artifact
C. Peritoneal nodule
D. Twinkle artifact
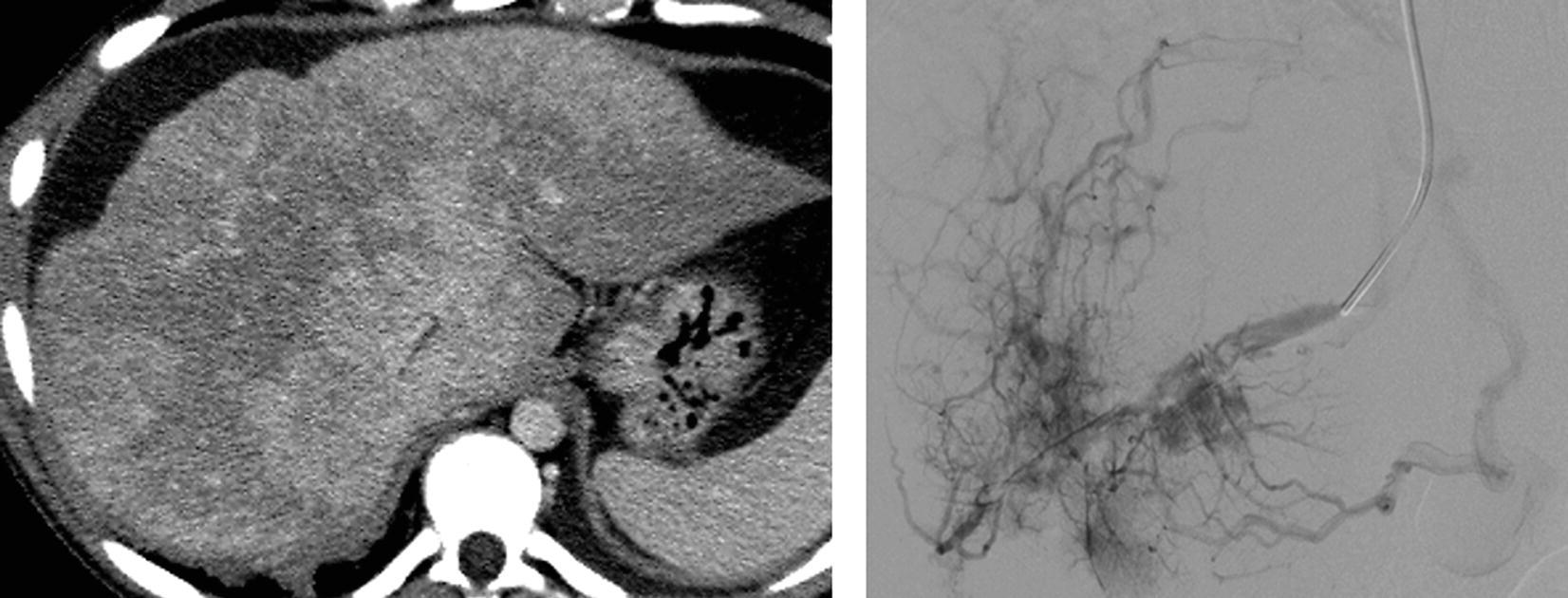
11 A 22-year-old patient presents with abdominal pain. A venous phase CT and hepatic venogram are shown. Which of the following is the most common known etiology of this disease process?
A. Thrombophilia
B. Viral hepatitis
C. Alcohol abuse
D. Congenital defect
For the patients in questions 12 to 15, select the most likely diagnosis (A to F). Each option may be used once or not at all.
A. Von Meyenburg complex
B. Pyogenic abscess
C. Biliary cystadenoma/cystadenocarcinoma
D. Peritoneal carcinomatosis
E. Polycystic liver disease in autosomal-dominant polycystic kidney disease
F. Subcapsular hematoma
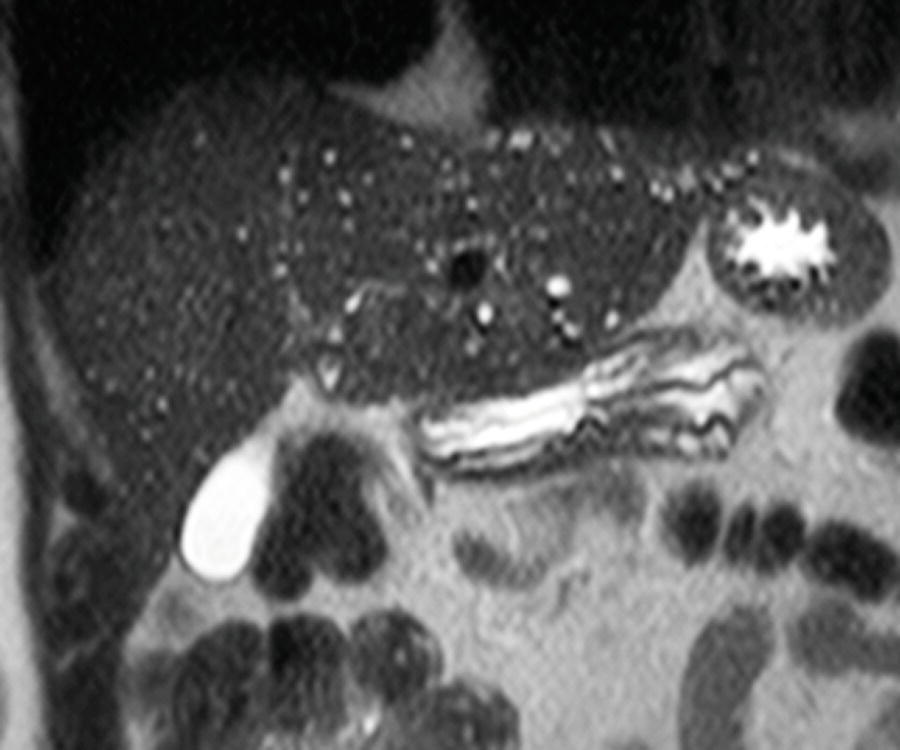
13 A woman with chronic renal failure, fatigue, and decreasing hematocrit.
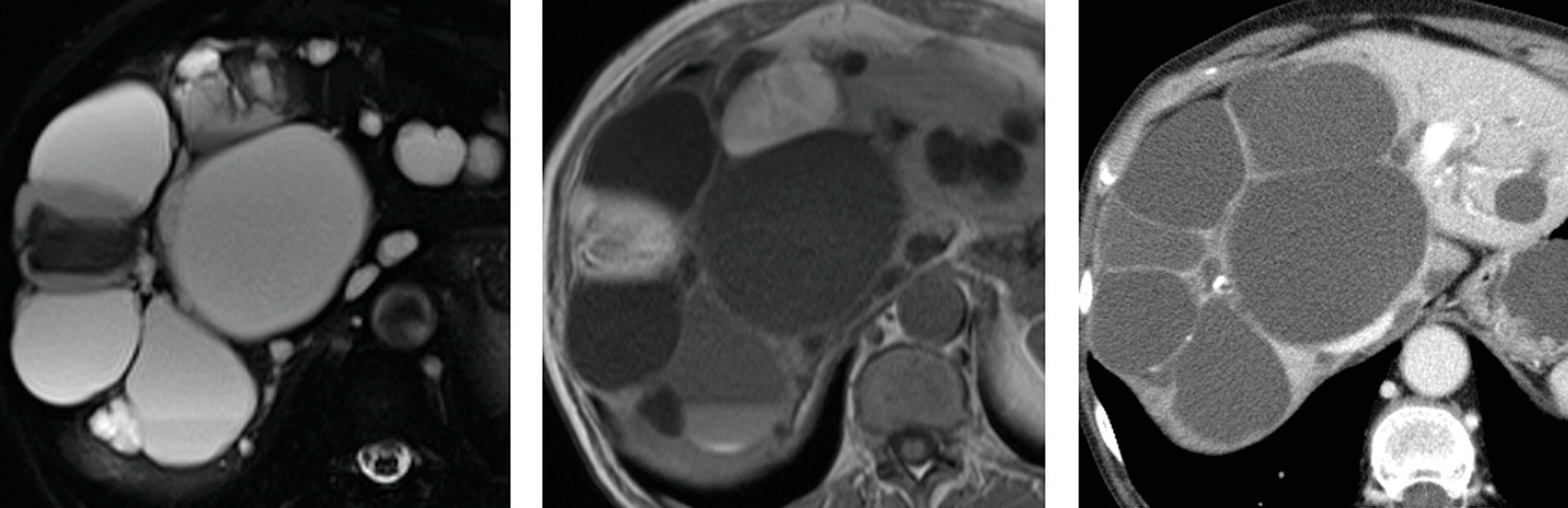
FS T2W, T1W MRI, and venous phase CT.
14 A 63-year-old man with pancreatic cancer status post common bile duct stent placement complains of worsening pain.
A. Right posterior hepatic notch sign
B. Macronodularity
C. Caudate lobe hypertrophy
D. Expanded gallbladder fossa sign
17 Regarding contrast agent selection for liver MRI, which of the following indications has the best consensus for the use of a hepatobiliary contrast agent such as gadoxetate disodium (Eovist—Bayer HealthCare) over a conventional extracellular contrast agent?
A. Assessing for residual or recurrent hepatocellular carcinoma after transarterial chemoembolization
B. Differentiating between focal nodular hyperplasia and hepatocellular adenoma
C. Confirming a hemangioma
D. Screening for hepatocellular carcinoma in a patient with hemochromatosis
18 A 54-year-old man undergoes MR imaging for evaluation of a liver mass. Among the choices listed, which is the most likely diagnosis?
Venous phase FS T1W+gad and T2W MRI.
A. Metastasis
B. Hemangioma
C. Simple cyst
D. Focal nodular hyperplasia
19a A 35-year-old man with end-stage renal disease underwent an abdominal ultrasound as part of preoperative evaluation for renal transplant. An MRI was performed to further evaluate an abnormal liver. The cause of the disease process revealed on these T1W GRE in-phase and out-of-phase images is most likely:
A. Viral hepatitis.
B. Blood transfusions.
C. Alcohol consumption.
D. Hereditary depositional disease.
19b Which of the following parameters would be the most effective for reducing T2* effect and susceptibility artifact?
A. Gradient-echo sequence and shorter TE
B. Gradient-echo sequence and longer TE
C. Fast spin-echo sequence and shorter TE
D. Fast spin-echo sequence and longer TE
20a A 46-year-old woman with breast ductal carcinoma in situ (DCIS) was found to have a liver lesion on breast MRI. Dedicated liver MRI was performed with a conventional extracellular contrast agent for further evaluation. What is the most likely diagnosis?
Top row: FS T2W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
A. Hemangioma
B. Metastatic breast cancer
C. Abscess
D. Hepatocellular carcinoma
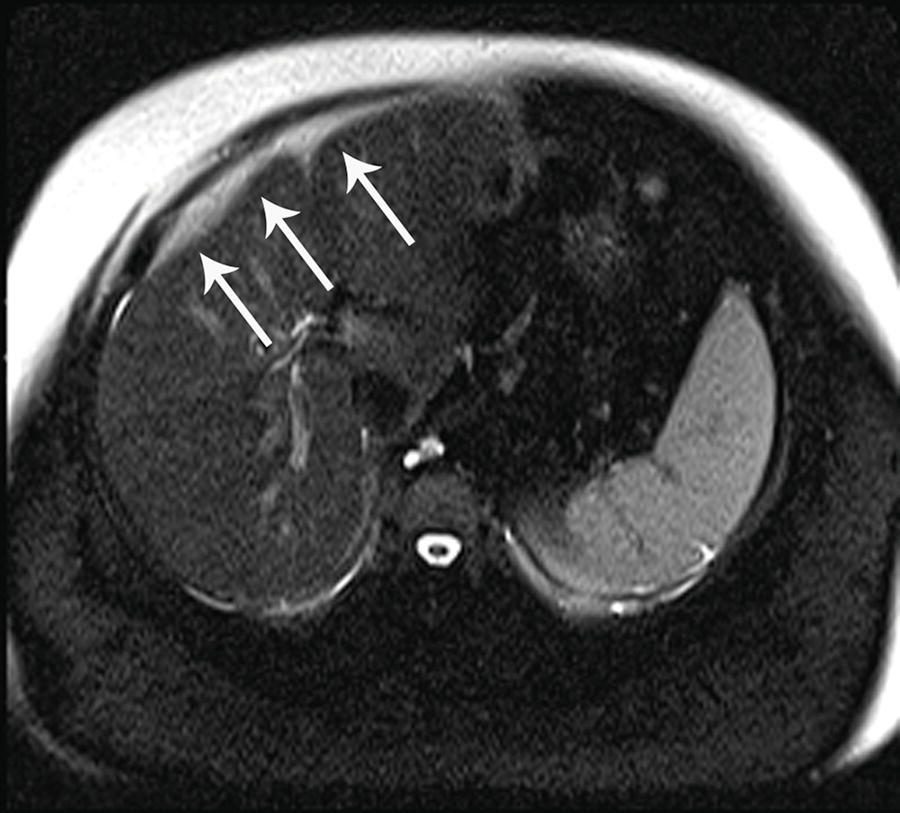
20b This is the arterial phase postcontrast T1W image from the previous case. What finding is indicated by the arrows?
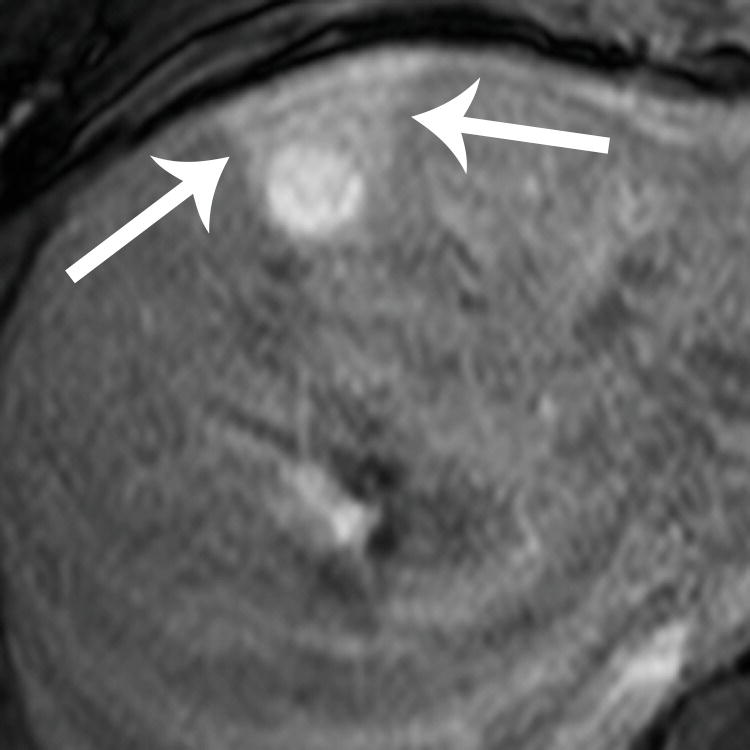
A. Poor fat saturation
B. Focal fatty sparing
C. Transient hepatic intensity difference (THID)
D. Hemorrhage
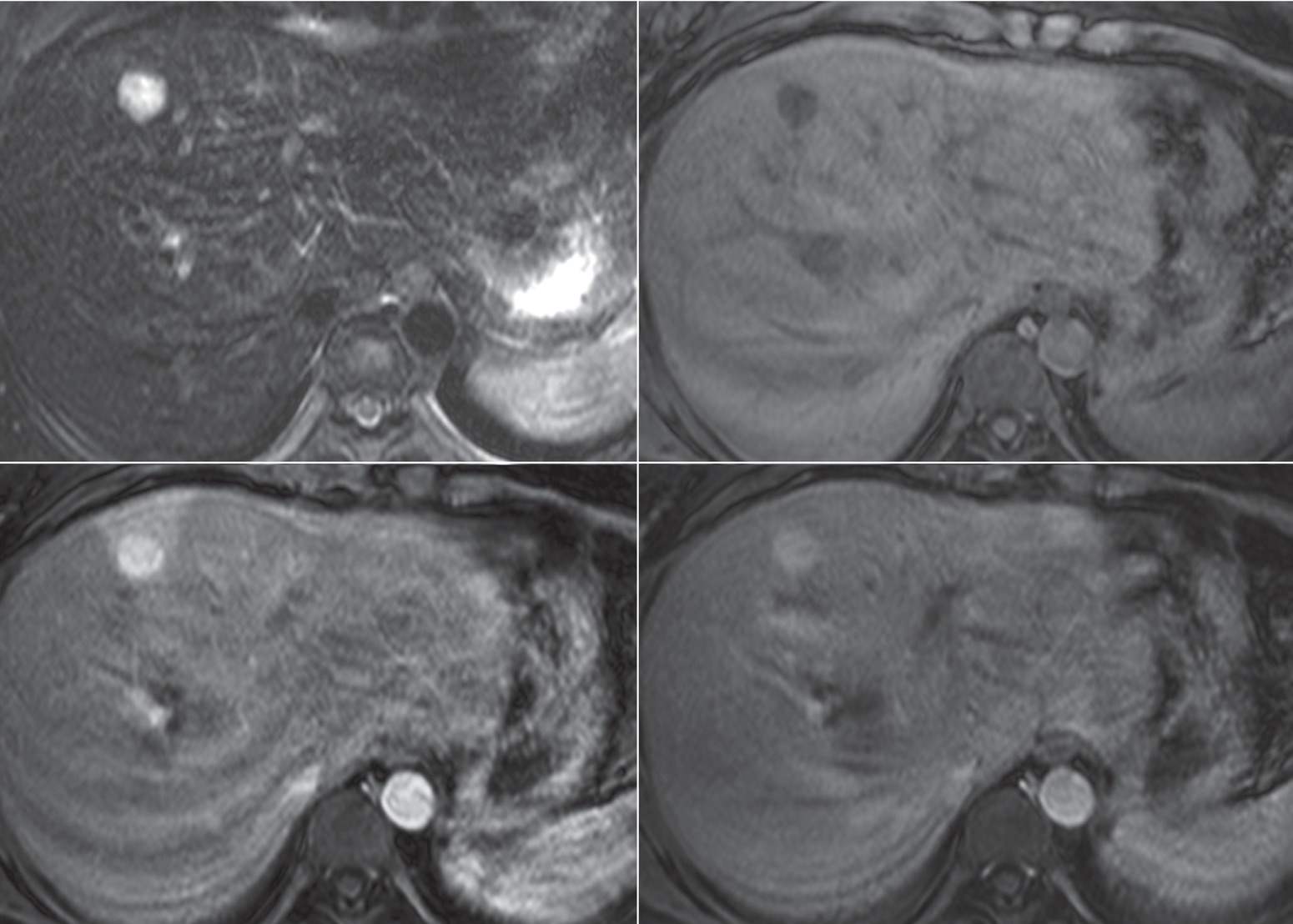
21 A 77-year-old man with chronic hepatitis B undergoes a screening MRI using conventional extracellular contrast agent. What is the most likely diagnosis?
Top row: In-phase and out-of-phase T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
A. Hepatocellular carcinoma
B. Hepatocellular adenoma
C. Angiomyolipoma
D. Nodular steatosis
22a A 19-year-old man was injured in a motor vehicle collision. Which statement is TRUE regarding the management of the liver findings on CT?
A. Partial hepatic resection is indicated for extent of laceration.
B. Angiography is indicated for embolization of a pseuodaneurysm.
C. No intervention is needed if patient is hemodynamically stable.
D. Percutaneous catheter placement is indicated for subcapsular hematoma.
22b The patient was hemodynamically stable and managed conservatively. Within 24 hours, the patient developed jaundice, which prompted a HIDA scan. What is the diagnosis?
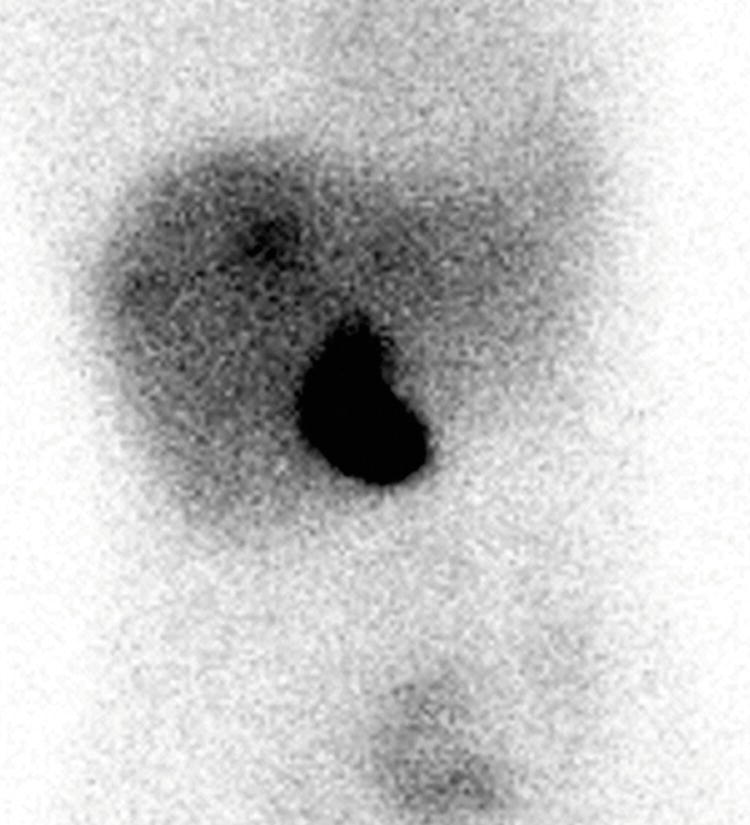
A. Intrahepatic bilomas
B. Intraperitoneal bile leak
C. Common bile duct obstruction
D. Gallbladder laceration
23 A 52-year-old woman undergoes a CT scan with images shown below. Imaging findings are consistent with:
A. Cholangiocarcinoma
B. Hemangioma
C. Lymphadenopathy
D. Portal vein occlusion
24a A 30-year-old woman is evaluated for a liver lesion that was incidentally noted at the time of a pelvic ultrasound. Which of the following statements is TRUE about the finding in the right lobe of the liver?
Top row: Noncontrast and arterial phase CT. Bottom row: Venous and delayed phase CT.
A. The finding demonstrates washout appearance and is most likely a malignancy.
B. The finding is likely a mass of hepatocellular origin.
C. The finding is likely a transient hepatic attenuation difference (THAD).
D. The finding demonstrates a central scar.
24b Hepatocellular adenomas in which of the following groups of patients have the highest risk of malignant transformation to hepatocellular carcinomas?
A. Women using oral contraceptives
B. Men
C. Patients with diabetes
D. Patients with steatosis in the background liver
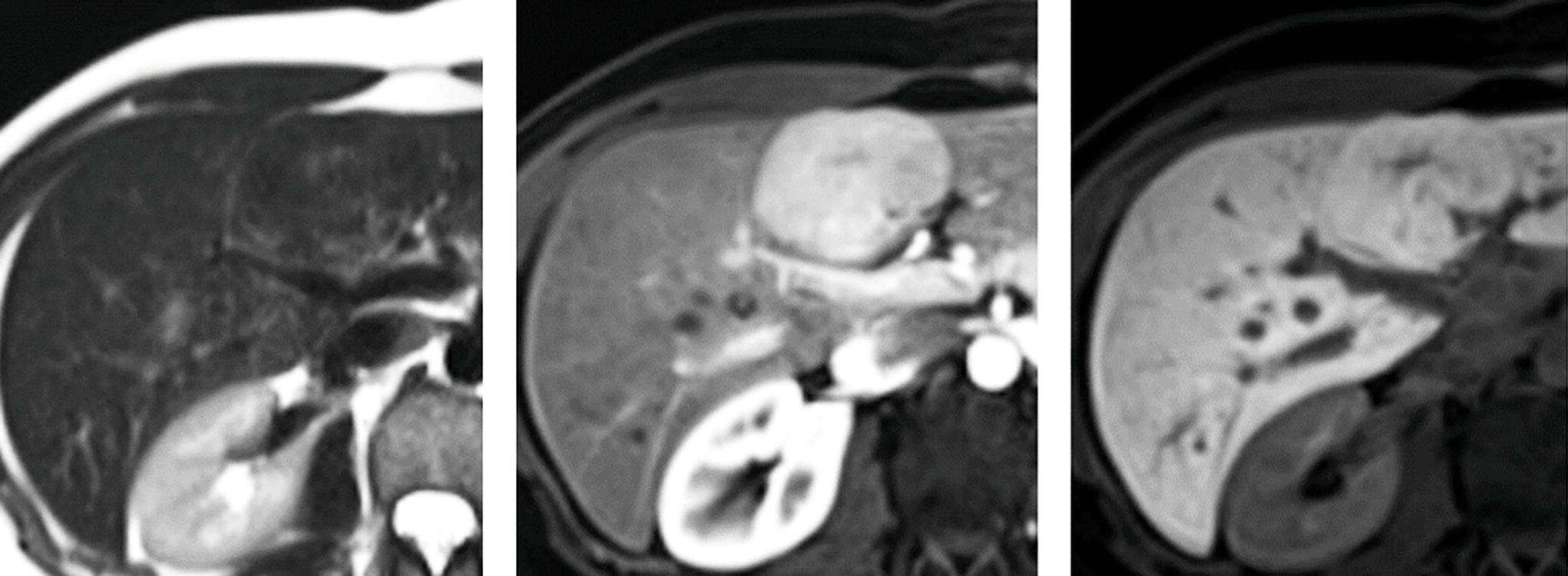
25a A 19-year-old woman was found to have elevated liver function tests. Workup included a liver MRI with hepatobiliary gadolinium contrast agent. Findings are most consistent with:
Top row: FS T2W and arterial phase FS T1W+hepatobiliary gad. Bottom row: Venous and hepatobiliary phase FS T1W+hepatobiliary gad.
A. Colon carcinoma metastasis
B. Giant cavernous hemangioma
C. Focal nodular hyperplasia
D. Fibrolamellar hepatocellular carcinoma
25b Which of the following statements is TRUE regarding fibrolamellar hepatocellular carcinoma (FHCC)?
A. Five-year survival is higher compared to conventional hepatocellular carcinoma.
B. Most patients are female.
C. The background liver is cirrhotic in the majority of cases.
D. There is a bimodal distribution affecting patients <40 and >60 years of age.
26 Which of the following is the most common benign liver tumor?
A. Hepatocellular adenoma
B. Focal nodular hyperplasia
C. Peliosis hepatis
D. Hemangioma
A. Congestive heart failure
B. Budd-Chiari syndrome
C. Arteriovenous malformation
D. Hepatic infarction
28 An MRI exam was performed in this 80-year-old woman with fever to further evaluate a liver mass seen on CT. What is the best explanation of findings on the (apparent diffusion coefficient) ADC map?
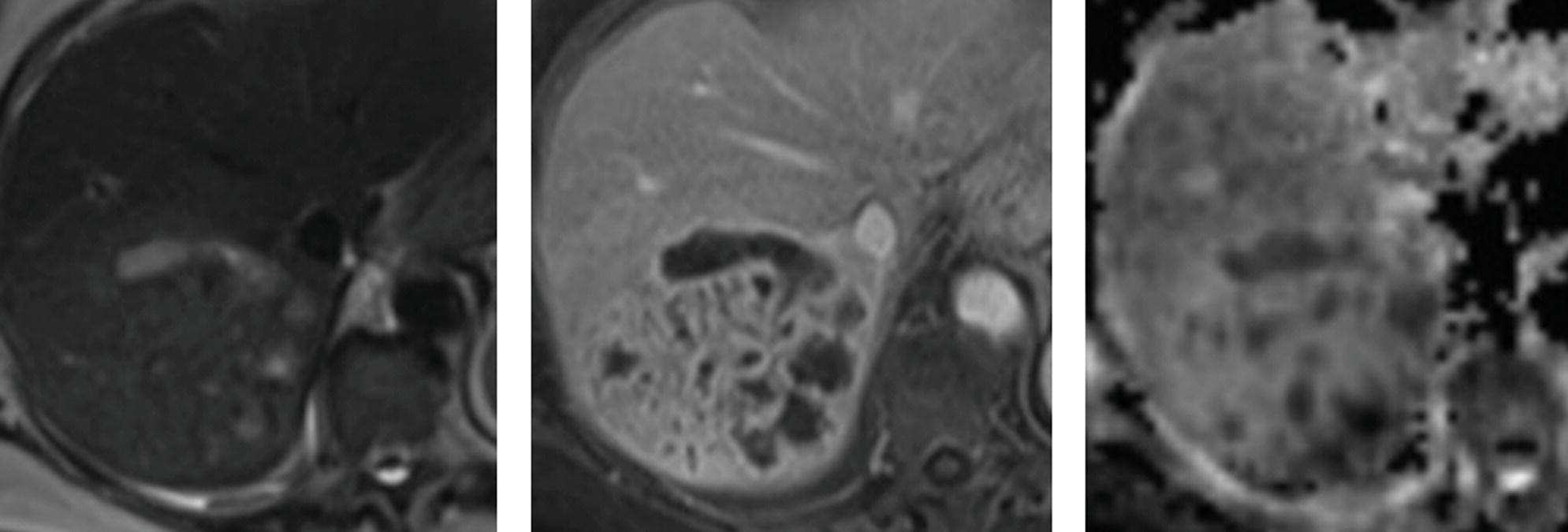
T2W, venous phase FS T1W+gad, and ADC map.
A. There is restricted diffusion in the enhancing soft tissue of this highly cellular neoplasm.
B. The foci of hypointensity on ADC map are due to gas.
C. There is restricted diffusion in the loculated fluid of this pyogenic abscess.
D. The foci of hypointensity on ADC map are due to iron deposition.
29 A 56-year-old woman presents with right upper quadrant pain and elevated liver function tests. Images from an MRI using conventional extracellular gadolinium contrast are shown below. What is the most likely diagnosis?
Top row: FS T2W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
A. Old infarct
B. Hemangioma
C. Ascending cholangitis
D. Cholangiocarcinoma
A. Portal vein thrombosis
B. Biliary ductal dilatation
C. Segmental fatty sparing
D. Liver laceration
31 A 68-year-old man with a history of primary sclerosing cholangitis is status post left hepatectomy for resection of a cholangiocarcinoma. The abnormality shown on the multiphase CT images below is associated with:
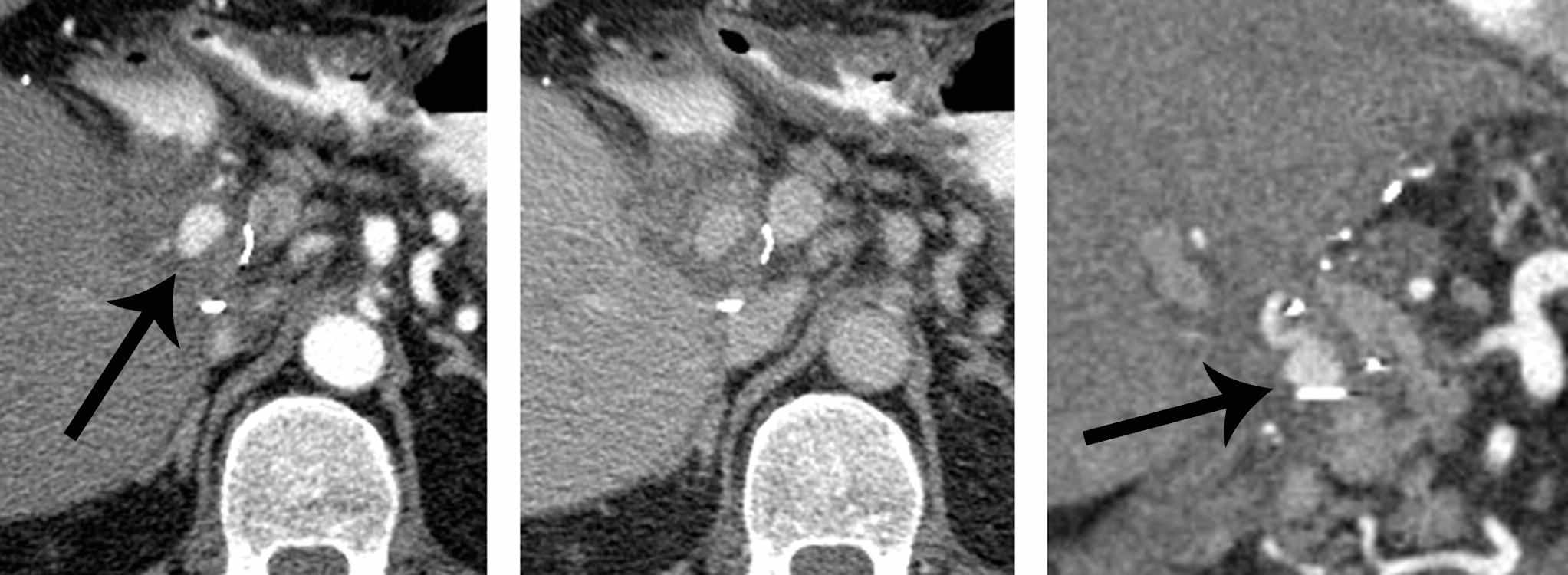
Axial arterial, axial venous, and coronal arterial phase contrast-enhanced CT.
A. Decreased platelet count
B. Decreased hematocrit
C. Elevated CA19-9 level
D. Elevated white blood cell count
32 A 22-year-old woman presented to the emergency department with malaise and elevated liver function tests after recent excessive alcohol consumption. An ultrasound was performed. What is the most likely diagnosis?

A. Ascending cholangitis
B. Acute hepatitis
C. Fungal microabscesses
D. Hemangiomas
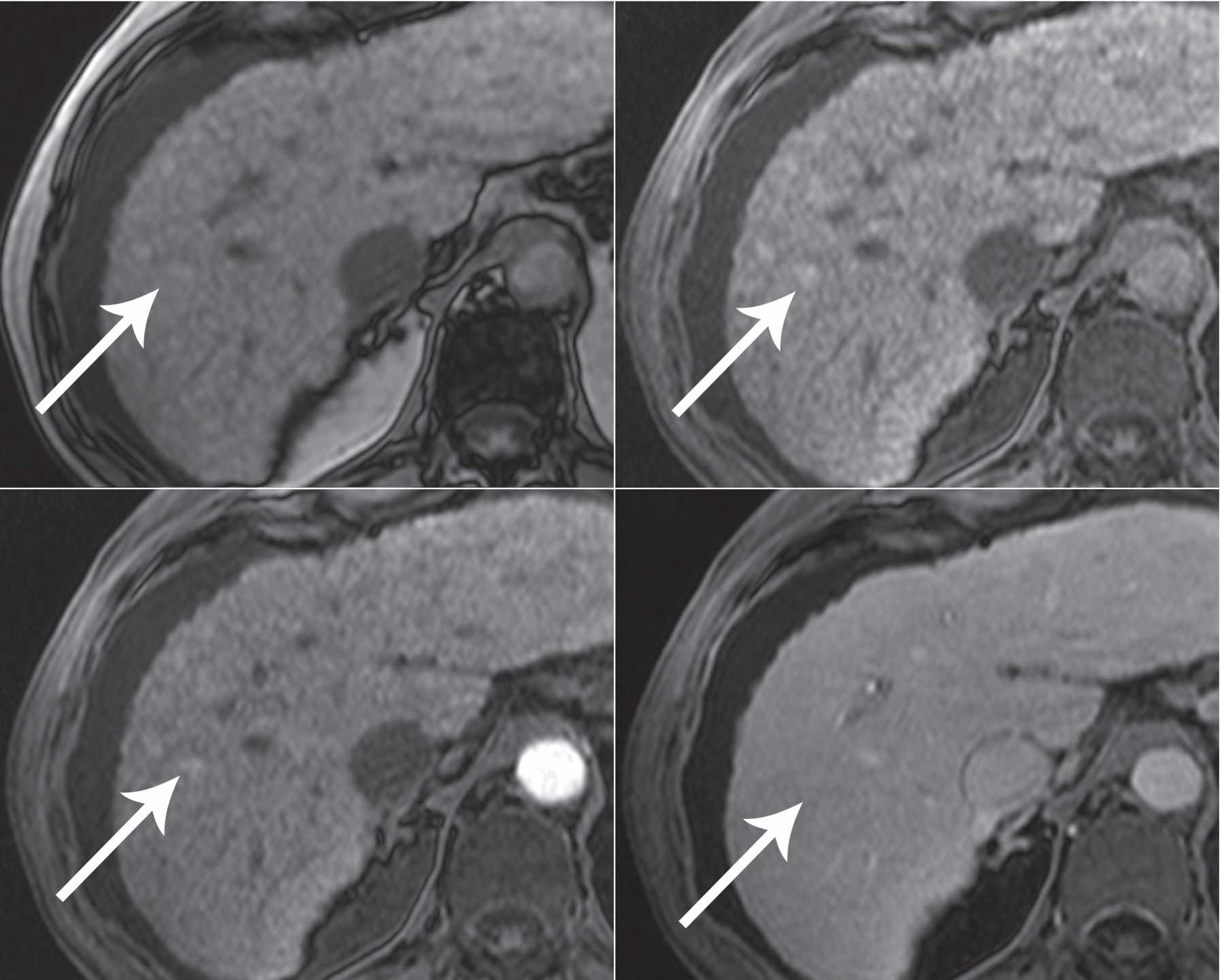
33a A 35-year-old woman with no history of chronic liver disease or underlying malignancy presents with abdominal pain. Based on the following MR images, what is the best description of the mass in the liver?
In-phase T1W, out-of-phase T1W, and FS T1W.
A. Fat-containing mass in the background of hepatic steatosis
B. Fat-containing mass in the background of hepatic hemosiderosis
C. Hemorrhagic mass in the background of hepatic steatosis
D. Hemorrhagic mass in the background of hepatic hemosiderosis
33b What is the most likely diagnosis of the mass in the previous question?
A. Focal nodular hyperplasia
B. Hepatocellular adenoma
C. Hepatocellular carcinoma
D. Metastatic disease
34 A 41-year-old woman who underwent a diagnostic procedure to evaluate suspected liver disease presents with acute severe epigastric pain. What finding is demonstrated involving the lateral segment left lobe on the CT?

A. Diffuse periportal edema
B. Focal fatty sparing
C. Subcapsular hematoma
D. Transient hepatic attenuation difference (THAD)
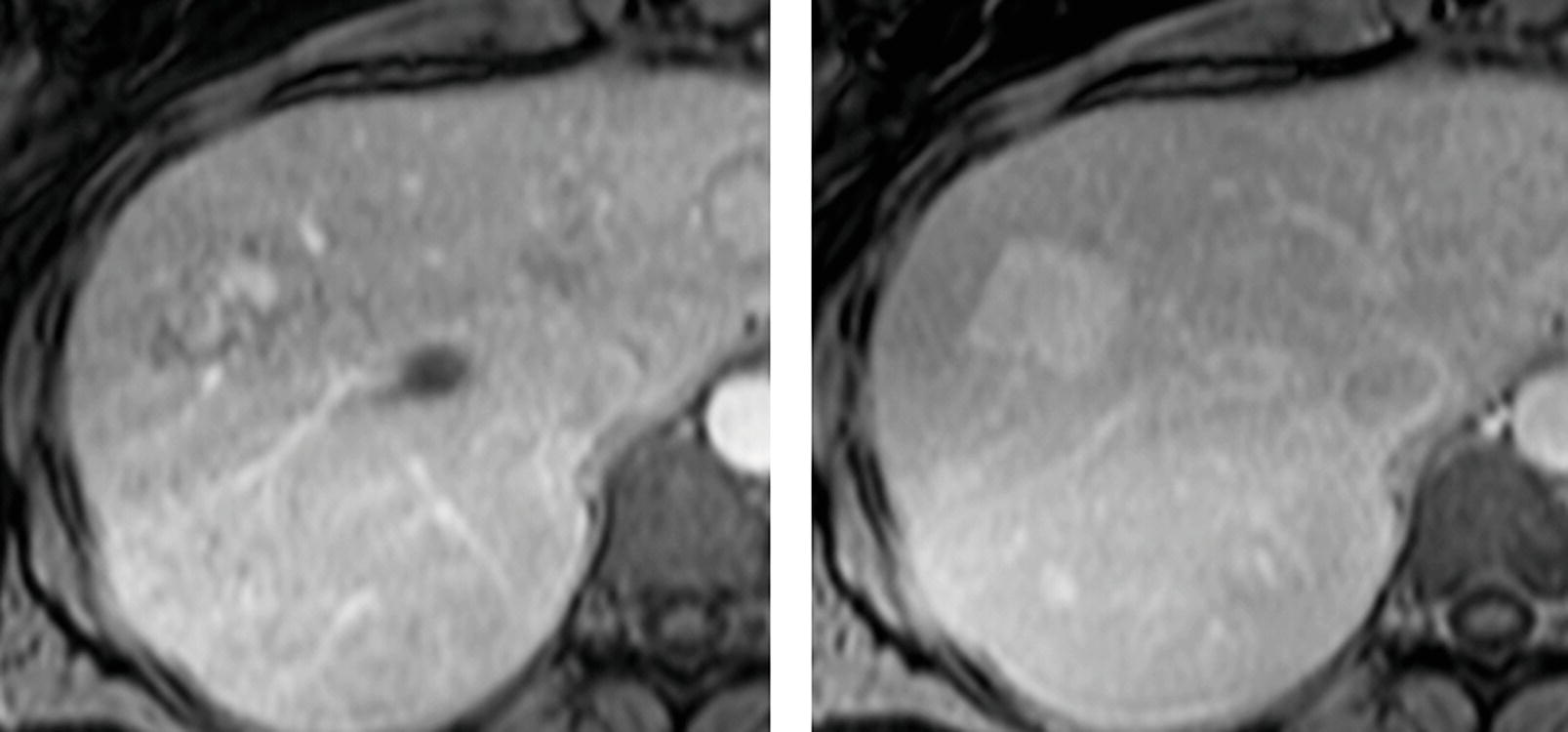
35 A 60-year-old man with cirrhosis underwent MRI exams 5 months apart. Arterial phase images of the current MRI exam are shown in the top row, and arterial phase images of the prior MRI exam are shown in the bottom row with a finding (arrow) in segment VII. The patient did not receive treatment between the exams. What is the most likely explanation for the appearance of the current exam in the top row?
A. The arterial phase on the current exam is not optimally timed for assessment of hypervascular neoplasms.
B. There has been spontaneous resolution of a dysplastic nodule.
C. There was a hepatocellular carcinoma that responded to treatment administered before both exams.
D. The finding the prior study was ghosting artifact from arterial pulsation no longer seen due to swapping of the phase- and frequency-encoding directions.
For the patients in questions 36 to 40, select the most likely underlying primary tumor (A to F) that is associated with the hepatic imaging findings. Each option may be used once or not at all.
A. Pancreatic ductal carcinoma
B. Neuroendocrine tumor
C. Non-small cell lung carcinoma
D. Breast carcinoma
E. Lymphoid tumor
F. Mucinous colorectal carcinoma
37 A 51-year-old man status post Whipple procedure.

Top row: Noncontrast and arterial phase. Bottom row: Venous and delayed phase.
38 A 41-year-old man status post liver transplant several months ago for cirrhosis and hepatocellular carcinoma. Arterial and venous phase CT as well as ultrasound images are shown.

39 A 77-year-old woman. Venous phase images are shown from two CT scans performed 12 months apart.
Initial scan and scan 12 months later after chemotherapy.
41 A patient with cirrhosis and hepatocellular carcinoma is undergoing evaluation for liver transplantation. Which of the following is a contraindication to transplantation according to the Milan criteria?
A. Encephalopathy
B. Refractory variceal hemorrhage
C. Malignant portal vein thrombus
D. Solitary HCC measuring 4 cm
42 The most common etiology of graft failure after liver transplant is
A. Posttransplant lymphoproliferative disorder
B. Vascular thrombosis
C. Biliary stricture
D. Rejection
43 A 63-year-old man with cirrhosis is status post CT-guided microwave ablation of a hepatocellular carcinoma in the right hepatic lobe. Two CT scans are shown. What is the most likely diagnosis?

Arterial phase CT scans 6 months after ablation and 14 months after ablation.
A. Hemangioma
B. Recurrent hepatocellular carcinoma
C. Abscess
D. Dysplastic nodule
A. Hemangioma
B. Simple cyst
C. Pulsatile flow artifact
D. Radiofrequency interference
45 A patient with a liver transplant was evaluated with ultrasound followed by angiography. The arrow indicates the location of spectral Doppler interrogation. What vascular complication is demonstrated?
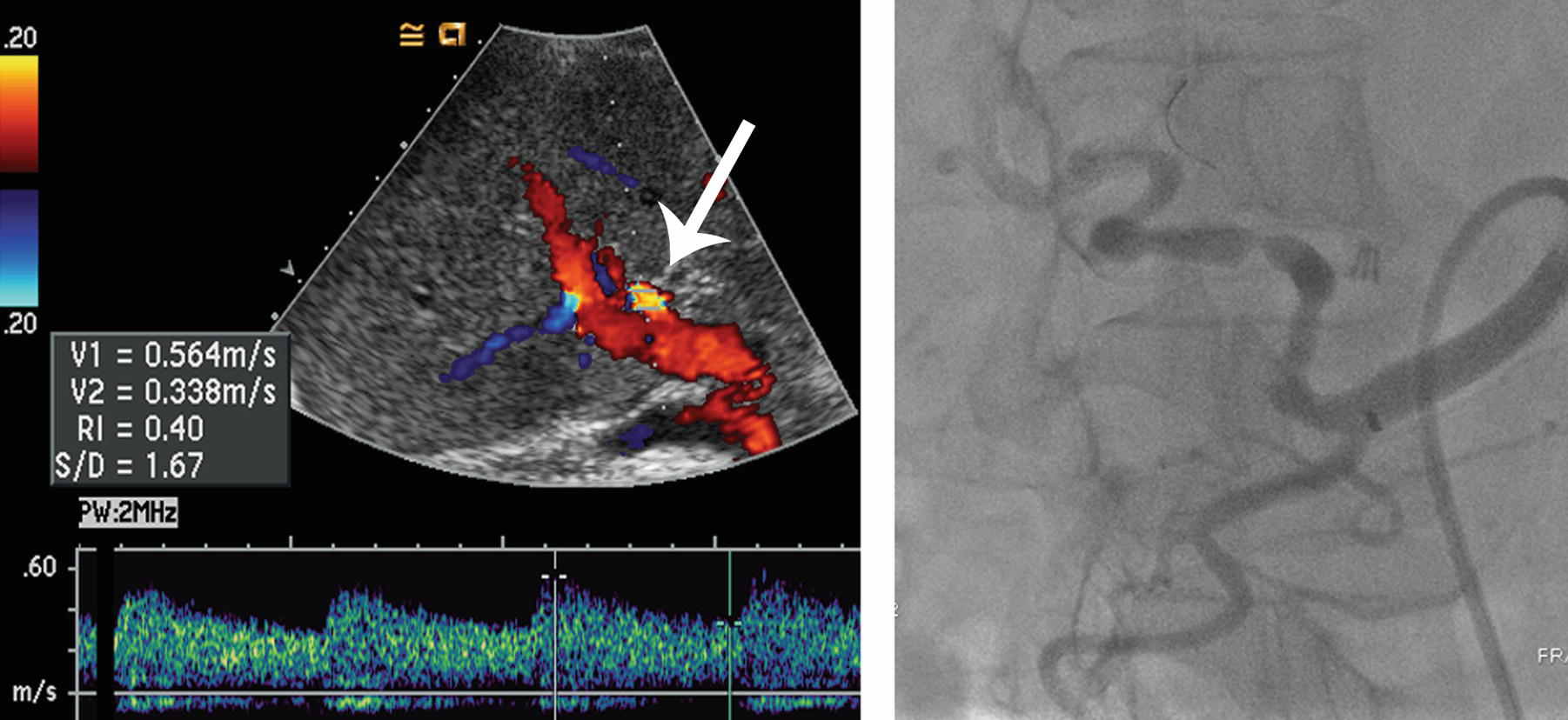
A. Hepatic artery stenosis
B. Portal vein thrombosis
C. Pseudoaneurysm
D. Arterioportal fistula
A. Kasabach-Merritt syndrome
B. Cushing syndrome
C. Carcinoid syndrome
D. Lambert-Eaton syndrome
For the patients in questions 47 to 50, select the most likely diagnosis (A to D) for the hepatic abnormalities. Each option may be used once, more than once, or not at all.
A. Siderotic nodule
B. Regenerative nodule, nonsiderotic
C. Nodular steatosis
D. Infarct
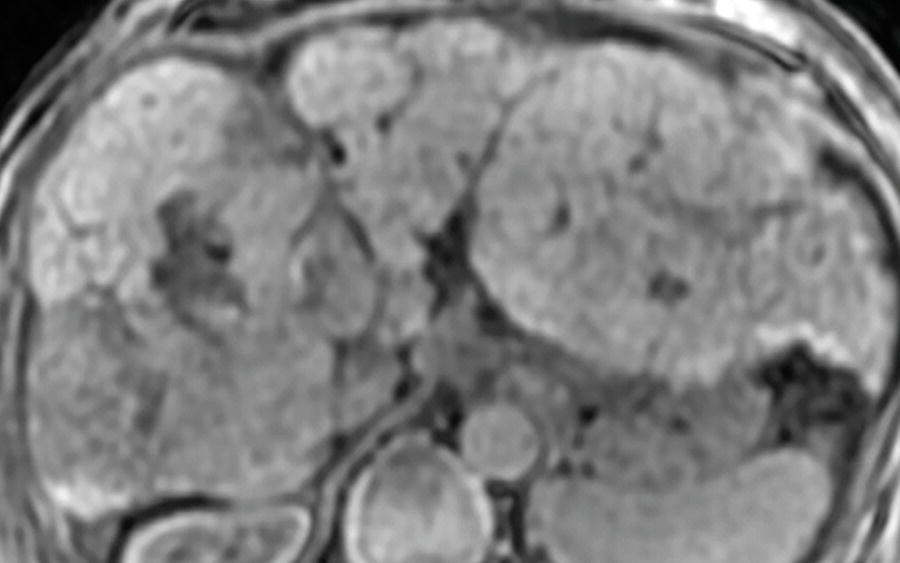
47 A 44-year-old woman with end-stage liver disease now with abdominal pain. Images from a CT scan and MRI are shown. A transjugular intrahepatic portosystemic shunt is partially visualized in the right lobe.
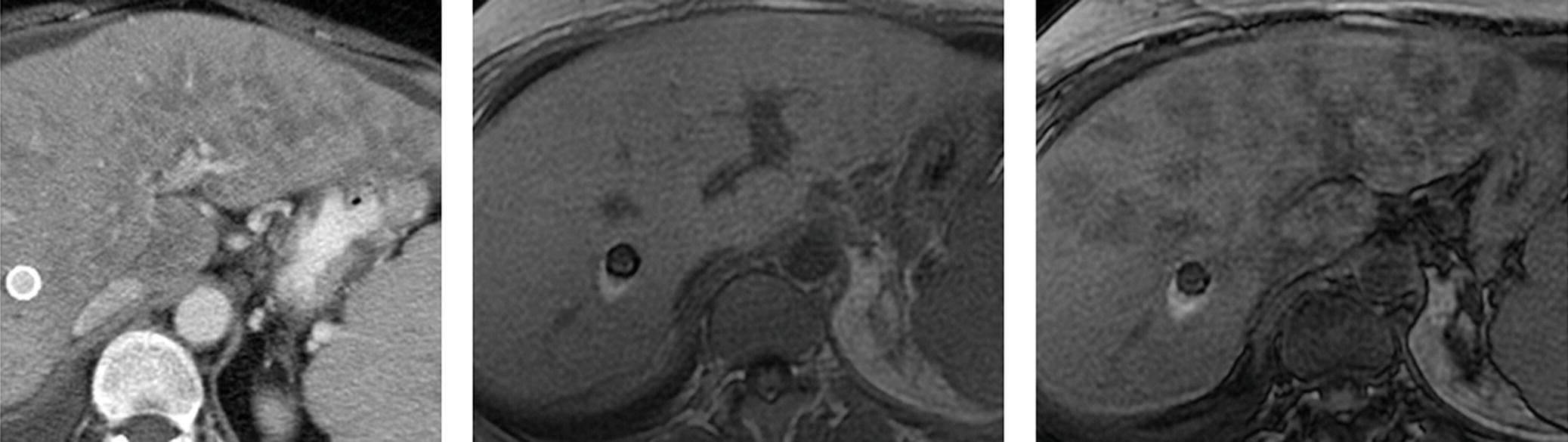
Venous phase CT, in-phase T1W MRI, and out-of-phase T1W MRI.
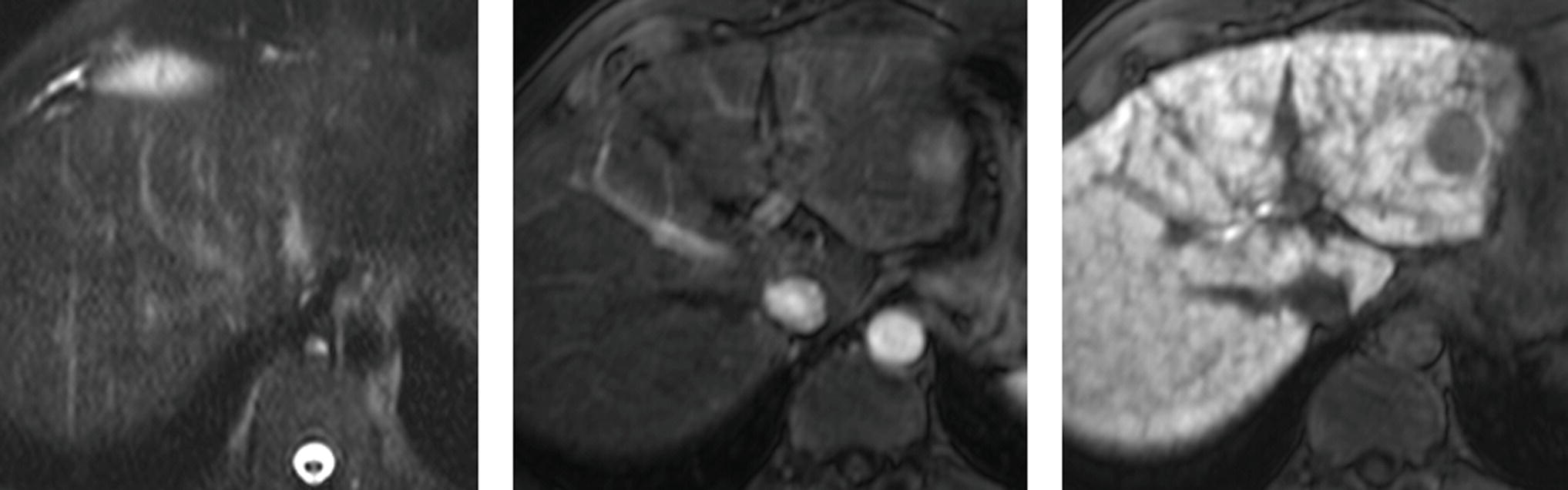
48 An MRI performed with conventional extracellular contrast agent is shown.
Top row: Out-of-phase T1W and FS T1W. Bottom row: Arterial and delayed phase FS T1W+gad.
49 A 39-year-old man with testicular cancer status post retroperitoneal nodal dissection. Postoperative course was complicated by hemoperitoneum. Images from two CT scans are shown.
Venous phase CT followed by noncontrast CT 1 month later.
50 A 53-year-old man with chronic hepatitis B infection.
Top row: In-phase and out-of-phase T1W. Bottom row: FS T2W and arterial phase FS T1W+gad.
A. Moiré fringes.
B. Focal fatty infiltration.
C. Ascites.
D. Uneven fat saturation.
52 A patient with cirrhosis underwent abdominal evaluation with ultrasound followed by CT. A spectral Doppler ultrasound image and two arterial phase CT images are shown. What is the finding?
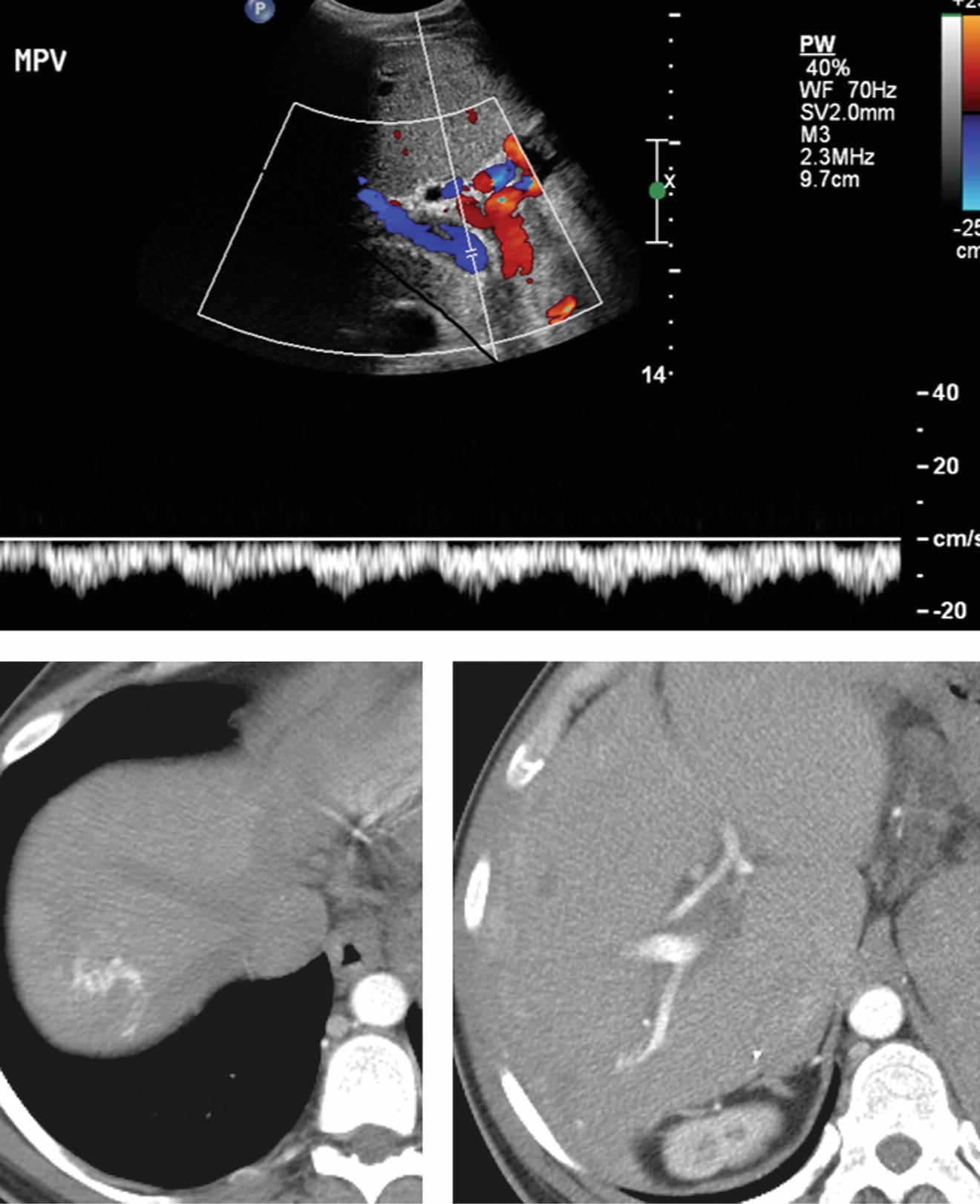
A. Hepatopedal flow in the portal vein
B. Respiratory variation in the portal vein
C. Arterioportal shunting
D. Cavernous transformation of the portal vein
53a A 46-year-old woman underwent MRI for multiple liver lesions found on ultrasound. Arterial and delayed phase FS T1W images from an MRI performed using conventional extracellular contrast agent are shown. This pattern of enhancement is most commonly identified with which of the following lesions?
A. Cavernous hemangioma
B. Peliosis hepatis
C. Lymphoma
D. Pseudoaneurysm
53b The organisms responsible for the most common form of peliosis hepatis seen in AIDS patients are species of:
A. Bartonella
B. Echinococcus
C. Ascaris
D. Cryptococcus
ANSWERS AND EXPLANATIONS
1 Answers: A4; B6; C7; D3; E1; F10; G2; H11; I9; J8; K5; L12.
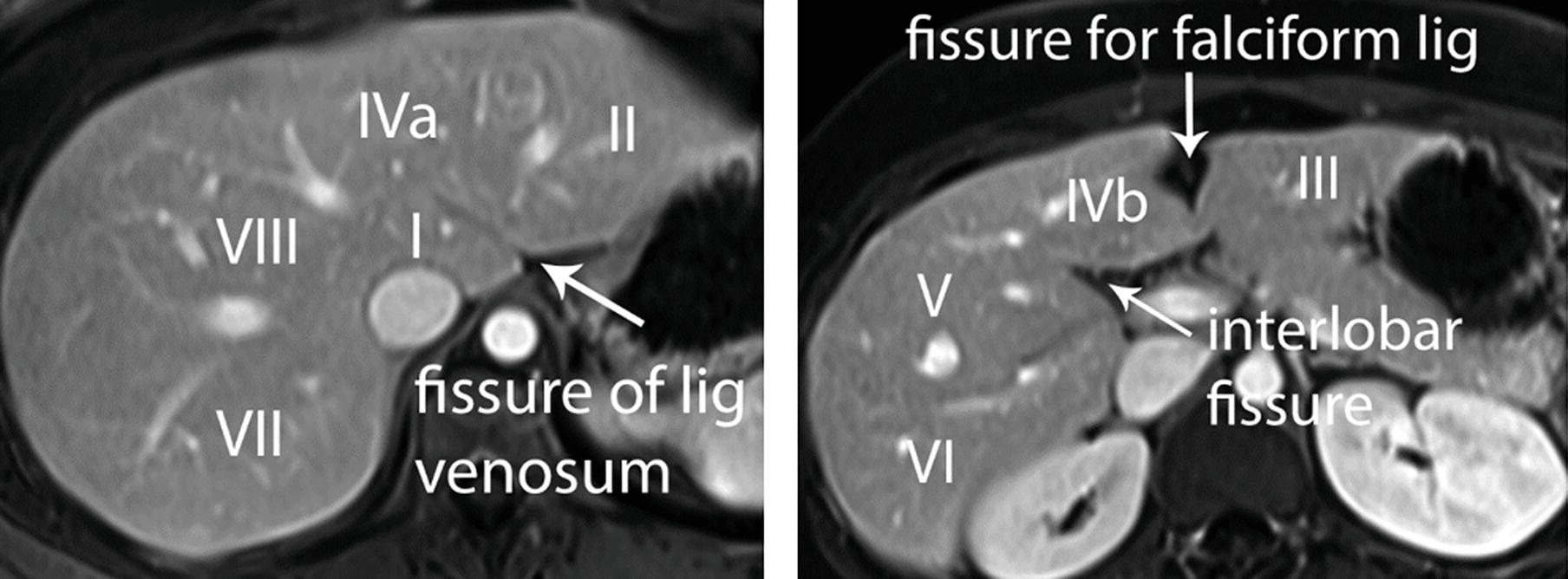
An understanding of hepatic lobar and segmental anatomy is essential in reporting to aid treatment planning. The liver is divided into right, left, and caudate lobes. The right lobe is subdivided into anterior and posterior segments and the left lobe into medial and lateral segments. The main hepatic veins are located in between segments of the liver. The portal triads (composed of the portal veins, hepatic arteries, and bile ducts) are located within segments of the liver. The Bismuth-Couinaud system is commonly used to provide a segmental nomenclature for localizing focal hepatic lesions. Vertically oriented planes along the right, middle, and left hepatic veins are maintained. These vertical planes intersecting a horizontal plane at the level of the right and left portal veins separate the liver into nine segments.
Segment I is the caudate lobe, located posterior to the fissure for the ligamentum venosum. Functionally, it is an autonomous part of the liver and has a separate blood supply, venous drainage, and biliary drainage.
The fissure for the ligamentum venosum is a coronally or obliquely oriented well-defined fissure. A normal variant accessory or replaced left hepatic artery from the left gastric artery can be seen running through this fissure.
The interlobar fissure (fissure of the gallbladder) separates the right and left lobes.
The fissure for the falciform ligament (fissure for the ligamentum teres) is located in the inferior aspect of the left hepatic lobe. The remnant umbilical vein “recanalizes” in the setting of portal hypertension and can be seen running through this fissure.
References: Boll DT, Merkle EM. Liver: normal anatomy, imaging techniques, and diffuse diseases. In: Haaga JR, Lanzieri CF, Gilkeson RC (eds). CT and MRI imaging of the whole body, 5th ed. Philadelphia, PA: Elsevier, 2009:1953–2040.
Ding A, Kulkarni N, Fintelmann FJ, et al. Liver: normal anatomy and examination techniques. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier Saunders, 2015:1471–1497.
2 Answer D.The liver is diffusely hyperdense in this patient with cardiac disease. Normal density is 45 to 65 HU on a noncontrast CT scan obtained with conventional kVp of 120. At visual inspection, it should appear similar to the spleen, which is about 35 to 55 HU. Diffuse hepatic hyperdensity can be caused by iodine deposition in patients treated with the cardiac antiarrhythmic drug amiodarone, which is 37% iodine by weight. This hyperdensity does not always indicate toxicity, and patients may be asymptomatic. However, if injury is severe, the patient may develop steatosis and cirrhosis. If there is pulmonary involvement, interstitial fibrosis and high-density pulmonary opacities may be seen.
Other causes of diffuse hepatic hyperdensity include hemochromatosis (iron deposition), Wilson disease (copper deposition), gold therapy, and glycogen storage disease. Thorotrast was associated with deposition of high density in a characteristic reticular pattern within the liver and spleen. The use of Thorotrast, a radioactive contrast agent, was discontinued in the 1950s when it was discovered to be carcinogenic. Total parenteral nutrition and radiation therapy are more commonly causes of steatosis and decreased liver density. Hepatorenal syndrome is unrelated to liver hyperdensity. It refers to renal failure caused by cirrhosis or fulminant hepatitis, leading to portal hypertension and ascites.
References: Coy, DL, Kolokythas O. Chapter 9: Liver and biliary. In: Lin E, Coy DL, Kanne JP (eds). Body CT: the essentials. New York, NY: McGraw-Hill, 2015.
Morgan T, Qayyum A, Gore RM. Chapter 89: Diffuse liver disease. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1629–1675.
3 Answer A.MRI is the imaging modality of choice to evaluate focal hepatic lesions, as reflected in the ACR Appropriateness Criteria. This series of questions reviews the classic appearances of some primary hepatic tumors on MRI. There is a well-circumscribed lesion in hepatic segment VII, which is very bright on the T2W image approaching signal intensity of cerebrospinal fluid, consistent with the “light bulb” sign. The mass demonstrates peripheral, nodular, discontinuous enhancement, followed by centripetal fill-in on delayed phase. These features are diagnostic for cavernous hemangioma. Fill-in may be partial or complete in hemangiomas. Hemangiomas are dilated venous channels with hepatic arterial supply. The great majority are asymptomatic and require no follow-up or treatment.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Cogley JR, Miller FH. MR imaging of benign focal liver lesions. Radiol Clin North Am 2014;52:657–682.
4 Answer D.This mass is a hepatocellular carcinoma (HCC). Signal intensity of the mass in segment VIII is similar to surrounding liver on both noncontrast T1W and T2W images, a clue that the tumor may be of hepatocellular origin (i.e., an HCC, focal nodular hyperplasia, or hepatocellular adenoma). The mass enhances on the arterial phase and demonstrates washout appearance as well as capsule appearance on delayed phase. These features are classic for HCC in this patient with cirrhosis. Additional imaging features that may be also present in HCC are intralesional fat, restricted diffusion, and portal vein tumor thrombus.
MRI is the most sensitive and specific imaging modality for the diagnosis of HCC. Awareness of patient demographics and clinical history is critical in the evaluation of hepatic lesions. In the presence of cirrhosis, a high index of suspicion for HCC should be maintained for any enhancing liver lesion. Washout appearance is an important imaging feature in the identification of classic HCC. A mass demonstrates washout appearance if it initially appears iso- to hyperintense to surrounding liver and then appears hypointense to surrounding liver on a later phase. “Washout” is often a misnomer because this appearance is predominantly due to increase in enhancement of the surrounding liver rather than loss of signal intensity by the mass itself.
References: ACR Appropriateness Criteria: Liver lesion— initial characterization. American College of Radiology website. https://acsearch.acr.org/docs/69472/Narrative. Published 1998. Updated 2014. Accessed April 4, 2015.
Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: Part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology 2014;273(1):30–50.
5 Answer E.This neoplasm is a mass-forming cholangiocarcinoma. The MRI demonstrates a large mass that shows sparse early enhancement and then heterogeneous progressive enhancement on later phases. Delayed enhancement is a feature suggesting a desmoplastic tumor such as a cholangiocarcinoma. Its hypointensity is very distinct from the surrounding liver parenchyma on T1W imaging, a clue that the tumor may not be of hepatocellular origin.
Cholangiocarcinoma is a malignant tumor arising from the biliary tree and represents the second most common primary malignancy of the liver. It can be categorized into three types based on morphology: mass-forming, periductal infiltrating, and intraductal growth types. Mass-forming cholangiocarcinoma may be seen with or without biliary ductal dilation. There may be associated hepatic capsular retraction, satellite nodules, and vascular encasement. It can be mistaken for a hemangioma due to its progressive delayed enhancement but lacks the well-defined puddles of peripheral discontinuous nodular enhancement seen with cavernous hemangiomas. In addition, the mass lacks the characteristic “light bulb” T2 hyperintensity of a hemangioma.
References: Chung YE, Kim MJ, Park YN, et al. Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics 2009;29(3):683–700.
Sainani NI, Catalano OA, Holalkere NS, et al. Cholangiocarcinoma: current and novel imaging techniques. Radiographics 2008;28(5):1263–1287.
6 Answer C.This patient has a focal nodular hyperplasia (FNH). There is an arterial-enhancing mass which retains contrast agent at 20 minutes on this MRI performed with Eovist hepatobiliary contrast agent. The mass is isointense on precontrast T2W image with exception of the small central scar, which is classically T2 hyperintense. All of the other answer choices are typically hypointense to the liver on the hepatobiliary phase.
If a conventional extracellular contrast agent (not shown here) is used, homogeneous arterial enhancement is seen, classically followed by venous and delayed phase isointensity. A prominent feeding vessel extending toward the central scar is sometimes identified on arterial phase. The central scar may enhance on the delayed phase when conventional extracellular contrast is used. Focal nodular hyperplasia is a benign mass representing a heptaocellular hyperplastic response to a pre-existing arterial malformation. It is most common in women of reproductive age. In 20% of cases, there are multiple lesions.
Differentiation from hepatocellular adenoma (HCA), another benign hypervascular hepatocellular tumor found in young women, is important as no other treatment is required for FNH, while HCA may require follow-up or intervention for hemorrhage, or rarely, malignant transformation. MRI with hepatobiliary contrast agent has been found to be highly sensitive and specific for differentiating FNH and HCA in this patient population. Because FNH contains normal functioning hepatocytes, it accumulates hepatobiliary contrast agent and remains iso- to hyperintense to the liver on 20-minute hepatobiliary phase images. In contradistinction, HCAs are hypointense on hepatobiliary phase.
References: Khosa F, Khan AN, Eisenberg RL. Hypervascular liver lesions on MRI. AJR Am J Roentgenol 2011;197(2):W204–W220.
Silva AC, Evans JM, McCullough AE, et al. MR imaging of hypervascular liver masses: a review of current techniques. Radiographics 2009;29(2):385–402.
7 Answer D.This is the expected appearance of a hepatocellular carcinoma (HCC) on an MRI performed with hepatobiliary contrast agent. The mass in the left lobe of the liver shows arterial enhancement. It is dark compared to surrounding liver on the hepatobiliary phase. There is evidence of cirrhosis with bands of fibrosis which are also hypointense on hepatobiliary phase. Other hypervascular masses such as hemangioma, hepatocellular adenoma (HCA), focal nodular hyperplasia (FNH), and metastasis are significantly less common in the cirrhotic liver compared to the general population. The lesion is isointense to the liver on T2 images, with no evidence of “light bulb” T2 hyperintensity to suggest a hemangioma. This 51-year-old man is not in the right demographic for HCA or FNH, lesions which most commonly occur in premenopausal women.
The role of hepatobiliary contrast agents in the patients at risk for HCC continues to evolve. In general, isointensity or hyperintensity on hepatobiliary phase is reassuring, suggestive of a benign finding such as regenerative nodule, dysplastic nodule, or arterioportal shunt with transient hepatic intensity difference (THID). Borders of an HCC may appear more sharply marginated on hepatobiliary phase than on other sequences, helping in the delineation and measurement of heterogeneous, infiltrative lesions.
References: Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: Part II. Extracellular agents, hepatobiliary agents, and ancillary imaging features. Radiology 2014;273(1):30–50.
Jhaveri K, Cleary S, Audet P, et al. Consensus statements from a multidisciplinary expert panel on the utilization and application of a liver-specific MRI contrast agent (gadoxetic Acid). AJR Am J Roentgenol 2015;204(3):498–509.
8 Answer D.If a hepatobiliary agent such as gadoxetate disodium (Eovist—Bayer HealthCare) is used, hypointensity on the 20-minute hepatobiliary phase is considered an ancillary feature that favors HCC according to LI-RADS (Liver Imaging Reporting and Data System). Ancillary features may upgrade suspicion for hepatocellular carcinoma no higher than category LI-RADS category 4 (probably HCC). Some other ancillary features that would favor HCC include diffusion restriction, nodule-in-nodule architecture, intralesional fat, and growth less than threshold.
LI-RADS was developed by a multidisciplinary committee supported by the American College of Radiology (ACR) to standardize interpretation and reporting of multiphase CT and MRI exams of the liver. LI-RADS is applicable to the patient population with cirrhosis or chronic hepatitis B and/or C, who are at risk for hepatocellular carcinoma (HCC). The algorithm for LI-RADS version 2014 is an interactive graphic on the ACR Web site with definitions, descriptions, and examples. LI-RADS categories range from LR-1 (100% certainty that observation is benign) to LR-5 (100% certainty that observation is HCC). When an observation does not meet criteria for other categories, it is designated LR-3 indicating intermediate probability for HCC.
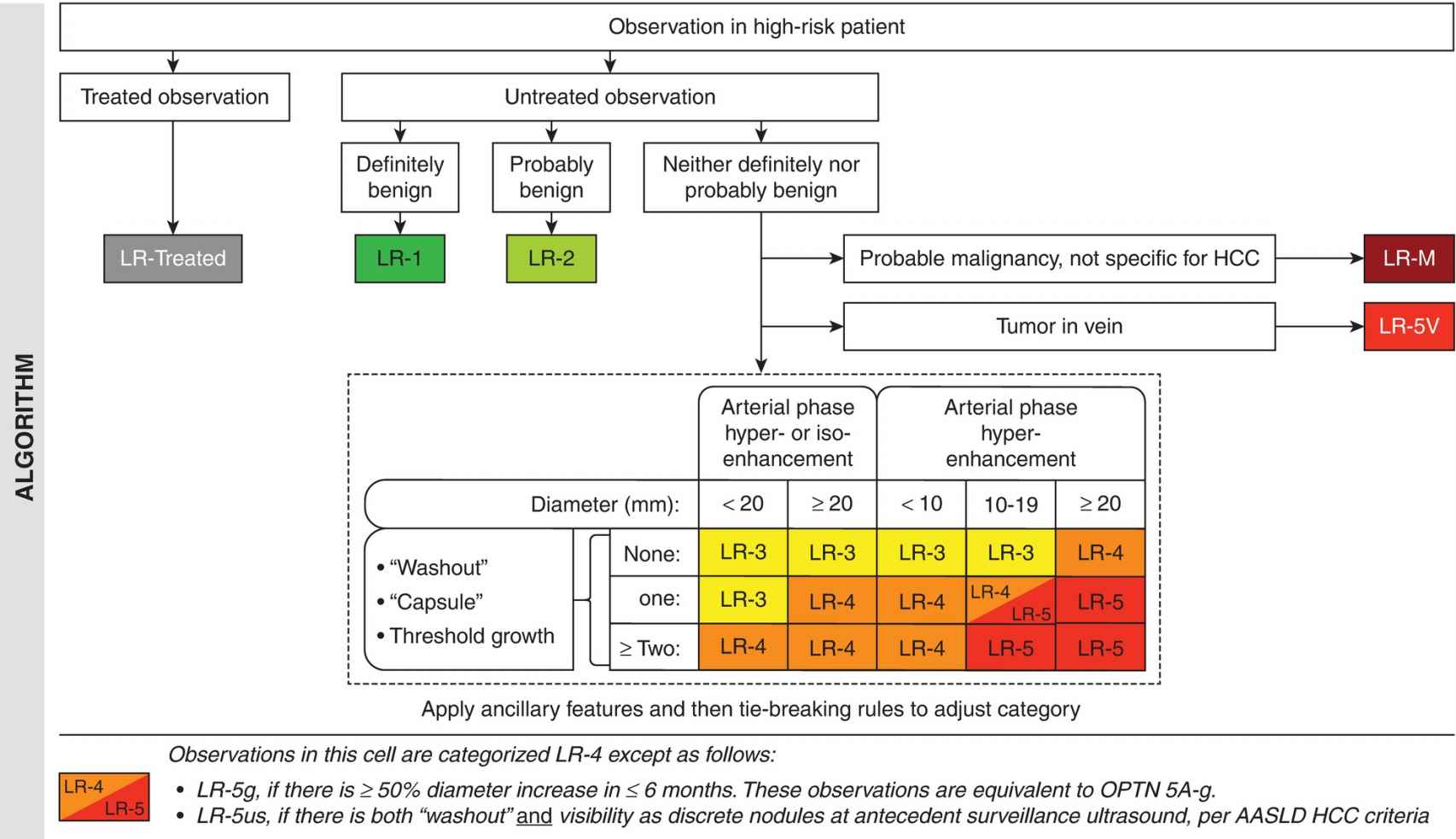
Reproduced with permission from the American College of Radiology. Liver Imaging Reporting and Data System version 2014. Accessed April 2015, from http://www.acr.org/Quality-Safety/Resources/LIRADS.
Major features for HCC in LI-RADS include “washout,” “capsule,” and threshold growth. Arterial enhancement and size thresholds are also included in major criteria, with masses ≥2 cm most worrisome. “Washout” and “capsule” specified in quotation marks (or washout appearance and capsule appearance) are the terms preferred by LI-RADS. This serves as a reminder that these terms are visual cues, which do not necessarily represent true loss of contrast enhancement on imaging or a true capsule at pathology.
Hepatobiliary phase hypointensity is not considered “washout.” On an MRI performed with a hepatobiliary contrast agent, it may only be appropriate to refer to washout appearance on the earliest venous phases in the dynamic portion of the exam (before 3 minutes) before the hepatobiliary phase dominates.
References: American College of Radiology. Liver Imaging Reporting and Data System version 2014. Accessed July 2015, from http://www.acr.org/Quality-Safety/Resources/LIRADS
Liu YI, Shin LK, Jeffrey RB, et al. Quantitatively defining washout in hepatocellular carcinoma. AJR Am J Roentgenol 2013;200(1):84–89.
9 Answer D.This hepatocellular carcinoma (HCC) is a large, infiltrative, heterogeneous mass with ill-defined margins. There is branching thrombosis of the right portal vein with patchy arterial enhancement consistent with tumor thrombus. Both the tumor and tumor thrombus show washout appearance on the delayed (equilibrium) phase. These features according to the LI-RADS algorithm are consistent with LR-5 category (definitely HCC) in this patient with cirrhosis. Portal vein tumor thrombus in a patient at risk for HCC increases the confidence level for HCC. A modifier for the thrombosis is added, making this case LR-5V (definitely HCC with tumor in the vein).
Portal vein thrombosis is found in greater than two-thirds of patients with infiltrative HCC. Tumor thrombus generally follows the imaging features of the primary HCC. Portal vein thrombosis can alter the perfusion of the liver and the tumor, presenting challenges in tumor diagnosis. Although identification of flow in the thrombus is specific for tumor thrombus, sensitivity is limited. Arterialization of the thrombus is detectable in fewer than 10% of cases. Significant expansion of the vein if seen favors tumor over bland thrombus.
Infiltrative HCC comprises about 13% of all HCC. Infiltrative HCCs have poor prognosis given their size and frequent association with tumor thrombus. Surgery decreases survival, so resection and transplantation are usually contraindicated. Response to systemic chemotherapy is poor. Intra-arterial chemoembolization may increase survival in a subset of patients with limited disease and adequate liver function.
References: American College of Radiology. Liver Imaging Reporting and Data System version 2014. Accessed April 6, 2015, from http://www.acr.org/Quality-Safety/Resources/LIRADS
Reynolds AR, Furlan A, Fetzer DT, et al. Infiltrative hepatocellular carcinoma: what radiologists need to know. Radiographics 2015;35(2):371–386.
10a Answer A.This incidentally discovered lesion in a young patient without significant past medical history has a low pretest probability for a malignancy. This lesion is in the periphery of the liver, well defined, and hyperechoic. The most likely diagnosis is a hemangioma. Color Doppler interrogation is not sensitive or specific for malignancy, since both benign and malignant lesions may have detectable or undetectable color Doppler flow.
The need for follow-up or definitive characterization of a liver lesion may depend on the patient age, underlying malignancy, presence of chronic liver disease, atypical hypoechoic or heterogeneous appearance, or request by the patient or physician. Regarding imaging management:
- Multiphase MRI is more sensitive and specific than CT. In addition, MRI does not involve ionizing radiation.
- Tc-99m red blood cell scan could be considered if a hemangioma requires confirmation and a low glomerular filtration rate precludes administration of MRI contrast (because of concerns about nephrogenic systemic fibrosis) or CT contrast (because of concerns about nephropathy). Lesions should be 2 cm or larger to be optimally evaluated on Tc-99m RBC scan. Increased uptake on the 1- to 2-hour blood pool images would be consistent with hemangioma.
- Follow-up ultrasound to document stability or no further workup may be appropriate for a lesion in young patients with low suspicion for malignancy.
References: ACR Appropriateness Criteria: Liver lesion—initial characterization. American College of Radiology website. https://acsearch.acr.org/docs/69472/Narrative. Published 1998. Updated 2014. Accessed April 4, 2015.
Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds.). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders; 2014:218–290.
10b Answer B.The finding indicated by the arrow represents a mirror artifact and should not be mistaken for a mass outside the liver. Mirror artifact is a type of reverberation artifact, with the mechanism depicted below.
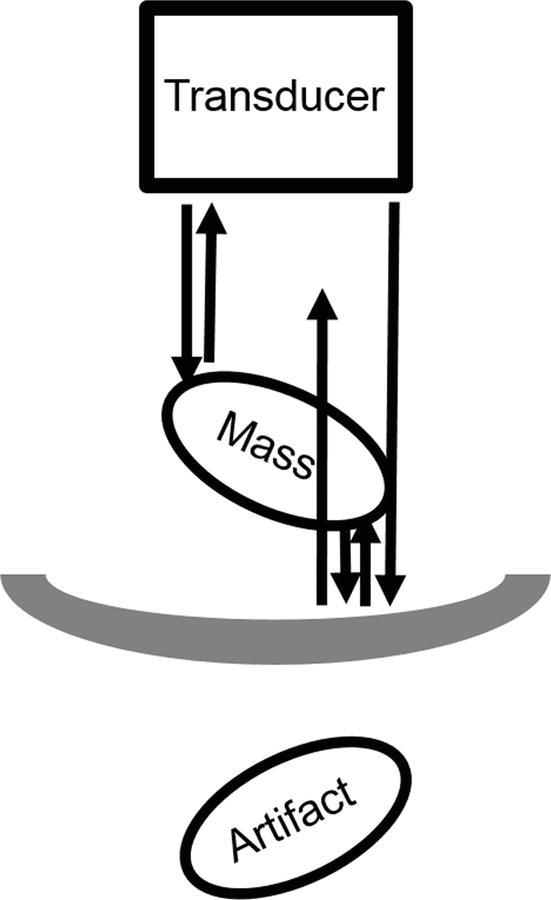
The beams that initially encounter the mass and return to the transducer are mapped correctly. However, some beams initially encounter the highly reflective surface of the diaphragm–air interface and reverberate between the diaphragm and the posterior margin of the mass before returning to the transducer. These late-returning echoes are erroneously mapped as a mirror image, farther away but equidistant from the diaphragm on the opposite side. Notice that the pseudolesion shows distortion and is not precisely the same shape or size as the true lesion.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds.). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Feldman MK, Katyal S, Blackwood MS. Ultrasound artifacts. Radiographics 2009;29(4):1179–1189.
11 Answer A.Axial contrast-enhanced image demonstrates a heterogeneous liver with a macronodular contour. There is enlargement and increased enhancement of the caudate lobe. The hepatic veins are not visualized. Hepatic venogram demonstrates “spider-web” collateral vessels, indicating hepatic venous obstruction consistent with Budd-Chiari syndrome (BCS).
The venous obstruction in BCS can occur from level of the small intrahepatic veins to the IVC. In the West, the typical patient is young and female. Primary BCS, in which the underlying obstruction originates from intrinsic venous sources, accounts for two-thirds of cases. These patients may have risk factors for thrombophilia including myeloproliferative disorders, factor V Leiden deficiency, antiphospholipid antibody syndrome, or protein C or S deficiency. In secondary BCS, obstruction results from an extrinsic source affecting the veins, such as metastatic lesions, abscesses, or trauma. Treatment options for BCS include anticoagulation/thrombolysis, angioplasty/stenting, and management of cirrhosis including portosystemic shunting and liver transplant.
BCS can be acute, subacute, or chronic. Imaging findings in the acute setting include thrombosed hepatic veins/IVC, ascites, and splenomegaly. Early in a multiphase scan, there may be peripheral hypovascularity and caudate hypervascularity. On subsequent phases of enhancement, a reversal or “flip-flop” of this pattern can be seen with peripheral hypervascularity and caudate hypovascularity.
Venous and delayed phase FS T1W MR images showing nodular regenerative hyperplasia in patient with BCS.
In the subacute to chronic setting, morphologic changes of cirrhosis as well as attenuation of the involved vessels can be seen. Patients can develop nodular regenerative hyperplasia (NRH), which represents growth of otherwise normal tissue that compensates for atrophy in other parts of the liver. Venous and delayed phase MR images below in a different patient with BCS demonstrate NRH, with large nodular areas of enhancement that can persist into the venous phase. There is no delayed washout appearance of these enhancing areas on delayed phase to suggest HCC, and these areas should not be mistaken for neoplasm.
References: Brancatelli G, Vilgrain V, Federle MP, et al. Budd-Chiari syndrome: spectrum of imaging findings. AJR Am J Roentgenol 2007;188(2):W168–W176.
Cura M, Haskal Z, Lopera J. Diagnostic and interventional radiology for Budd-Chiari syndrome. Radiographics 2009;29(3):669–681.
12 Answer C.The patient has findings suspicious for biliary cystadenoma (BCA) or biliary cystadenocarcinoma (BCAC), which may be considered a mucinous cystic neoplasm. There is an encapsulated, multiloculated cystic mass in the right lobe of the liver with thin as well as a few thicker enhancing septations. There is biliary ductal dilation in the left lobe in this case.
Lesions are often large at presentation, and calcifications may be present. Solid enhancing components would increase suspicion for cystadenocarcinoma. There is a female predominance, and patients may be asymptomatic or present with nonspecific symptoms. Features of BCA and BCAC overlap, but even if benign, resection should be considered as the risk of malignant transformation in BCAs is as high as 20%. Occasionally, ovarian-type stroma may be found at pathology. These lesions can be difficult to fully resect, and the rate of recurrence is up to 90%.
The differential diagnosis of a multiloculated encapsulated cystic lesion in the liver would include infections such as pyogenic abscess and hydatid (echinococcal) cyst. In this case, most of the cyst walls and septations are relatively thin, and there is no surrounding inflammation of the liver parenchyma to strongly suggest a pyogenic abscess. A form of intraductal papillary mucinous tumor (IPMN) that arises from the bile duct may have the appearance of a cystic liver mass with associated biliary ductal dilation as well.
References: Borhani AA, Wiant A, Heller MT. Cystic hepatic lesions: a review and an algorithmic approach. AJR Am J Roentgenol 2014;203(6):1192–1204.
Qian LJ, Zhu J, Zhuang ZG, et al. Spectrum of multilocular cystic hepatic lesions: CT and MR imaging findings with pathologic correlation. Radiographics 2013;33(5):1419–1433.
13 Answer E.The multiple renal cysts are not shown on these images, but among the choices in this patient with chronic renal failure, the most likely diagnosis is polycystic liver disease (PLD) in the setting of autosomal dominant polycystic kidney disease (ADPCKD). Some of the cysts are complicated by hemorrhage in this patient with decreasing hematocrit. The following T2W MR image from a different patient with ADPCKD shows the classic appearance with hepatic cysts and cystic replacement of the kidneys.
ADPCKD with renal and hepatic cysts.
When more than 10 hepatic cysts are identified, a fibropolycystic liver disease such as PLD could be considered. These cysts represent dilated abnormal bile ducts related to embryologic malformation of the ductal plate and no longer communicate with the biliary tree. Cysts are of variable sizes and have thin walls without enhancement. On MRI, cysts may be heterogeneous due to infection or hemorrhage. Management is generally supportive, although in some cases large cysts may be targeted for aspiration for symptomatic relief.
References: Borhani AA, Wiant A, Heller MT. Cystic hepatic lesions: a review and an algorithmic approach. AJR Am J Roentgenol 2014;203(6):1192–1204.
Brancatelli G, Federle MP, Vilgrain V, et al. Fibropolycystic liver disease: CT and MR imaging findings. Radiographics 2005;25(3):659–670.
14 Answer B.This case demonstrates the “double-target” sign of pyogenic (bacterial) hepatic abscess on CT. There is a hypodense center representing necrosis, a hyperdense inner rim of enhancing granulation tissue, and a hypodense outer rim of inflammatory edema. Gas may be seen internally as in this case. On ultrasound, abscesses may have a complex cystic appearance with internal debris and posterior acoustic enhancement, as demonstrated on the following image from a different patient.
Abscess with multiloculated appearance.
Pyogenic abscesses are the most common hepatic abscess in the United States, followed by fungal and amebic abscesses. This cancer patient with a history of biliary stenting and obstruction is at risk for development of cholangitis and hepatic abscess. Patients with history of surgery, trauma, and bacteremia are also at risk. Diverticulitis and appendicitis can cause pyogenic abscesses due to seeding via the portal venous system, but seeding is less common now due to rapid diagnosis and treatment of these diseases. Amebic abscesses tend to be unilocular and may appear similar to pyogenic abscess with thickened wall. Hepatic abscesses are associated with significant morbidity and mortality, and early intervention antibiotics and percutaneous drainage are indicated.
References: Borhani AA, Wiant A, Heller MT. Cystic hepatic lesions: a review and an algorithmic approach. AJR Am J Roentgenol 2014;203(6):1192–1204.
Qian LJ, Zhu J, Zhuang ZG, et al. Spectrum of multilocular cystic hepatic lesions: CT and MR imaging findings with pathologic correlation. Radiographics 2013;33(5):1419–1433.
15 Answer A.Findings are most consistent with biliary hamartomas, also known as von Meyenburg complex. There are numerous subcentimeter T2 hyperintense lesions scattered throughout the liver. Biliary hamartomas are typically of fairly uniform small size <15 mm, while simple hepatic cysts and polycystic liver disease are more variable in size as shown in question 13. Margins of biliary hamartomas may be angular, and enhancement is uncommon.
Biliary hamartomas are considered a fibropolycystic liver disease resulting from abnormal embryologic development of the biliary ductal plate. These lesions no longer communicate with the biliary ducts. Biliary hamartomas are benign, asymptomatic and do not require intervention. The differential diagnosis for widespread, small, cystic liver lesions includes simple hepatic cysts, microabscesses (typically fungal infection), and Caroli disease.
References: Anderson SW, Kruskal JB, Kane RA. Benign hepatic tumors and iatrogenic pseudotumors. Radiographics 2009;29(1):211–229.
Brancatelli G, Federle MP, Vilgrain V, et al. Fibropolycystic liver disease: CT and MR imaging findings. Radiographics 2005;25(3):659–670.
16 Answer B.The MRI in this patient with cirrhosis demonstrates a macronodular hepatic contour secondary to large regenerating nodules and intervening fibrosis. In addition to macronodularity, other imaging features that may be seen with cirrhosis are:
- Micronodular regenerating nodules
- Segmental atrophy (commonly the right lobe and medial segment of the left lobe)
- Segmental hypertrophy (commonly the caudate lobe and lateral segment of the left lobe)
- Right posterior hepatic notch sign (focal indentation of the posteroinferior surface of the right lobe at the level of the right kidney secondary to enlargement of the caudate lobe and atrophy of the right lobe)
- Expanded gallbladder fossa sign (increased fat in the pericholecystic area)
Delayed contrast enhancement is typical of fibrosis. There is no arterial enhancement. Fibrosis can be lattice-like with bridging or confluent in appearance (arrow) as shown on the following images from different patients.
Lattice-like bridging fibrosis and confluent fibrosis.
The cause of a patient’s cirrhosis or fibrosis usually cannot be determined based on imaging alone, but there may be clues to the underlying diagnosis:
- Biliary ductal beading could indicate primary sclerosing cholangitis as the cause.
- Caudate lobe hypertrophy and the right posterior hepatic notch sign are reportedly more common in alcoholic than viral induced cirrhosis.
- A pathognomonic “turtleback” or “tortoiseshell” pattern of periportal fibrosis with septal and capsular calcification has been described with schistosomiasis infection.
Cirrhosis diagnosed at biopsy may not be morphologically detectable on conventional imaging. More recent techniques that are being used to improve detection of cirrhosis include ultrasound and MR elastography to create maps of liver stiffness.
References: Dodd GD, Baron RL, Oliver JH, et al. Spectrum of imaging findings of the liver in end-stage cirrhosis. Part I. Gross morphology and diffuse abnormalities. AJR Am J Roentgenol 1999;173(4):1031–1036.
Faria SC, Ganesan K, Mwangi I, et al. MR imaging of liver fibrosis: current state of the art. Radiographics 2009;29(6):1615–1635.
17 Answer B.One of the most widely accepted indications for performing an MRI with a hepatobiliary contrast agent is differentiating between focal nodular hyperplasia (FNH) and hepatocellular adenoma (HCA). Hepatobiliary MRI contrast agents are being increasingly used for the evaluation of the liver. Conventional extracellular contrast agents used in CT and MRI are excreted by the kidneys. While hepatobiliary agents have some extracellular activity, allowing for some degree of dynamic assessment on arterial and portal venous phases, these agents are also taken up by hepatocytes with subsequent biliary excretion. Gadoxetate disodium (Eovist—Bayer HealthCare) is an agent that has moderate (50%) uptake by hepatocytes. Lesions without functioning hepatocytes appear hypointense on the 20-minute T1W hepatocyte phase images. There is biliary excretion and contrast can be seen in the ducts in the hepatobiliary phase.
The following two tables list clinical scenarios and rationales for selecting a hepatobiliary contrast agent versus a conventional extracellular contrast agent.
Potential Applications of Hepatobiliary Gadolinium-Based Contrast Agents
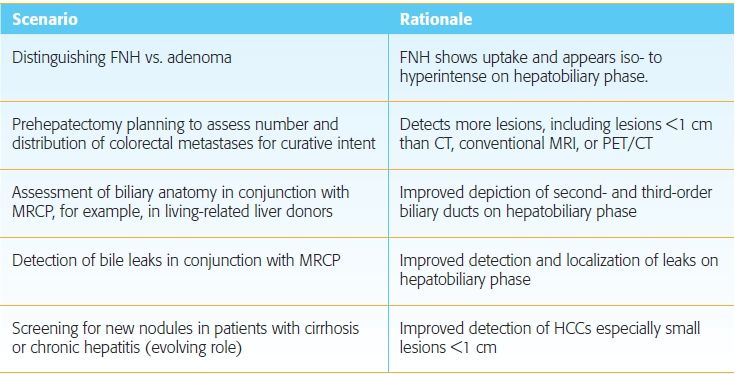
Scenarios in Which MRI or CT Using Conventional Contrast May Be Preferred
References: Jhaveri K, Cleary S, Audet P, et al. Consensus statements from a multidisciplinary expert panel on the utilization and application of a liver-specific MRI contrast agent (gadoxetic acid). AJR Am J Roentgenol 2015;204(3):498–509.
Seale MK, Catalano OA, Saini S, et al. Hepatobiliary-specific MR contrast agents: role in imaging the liver and biliary tree. Radiographics 2009;29(6):1725–1748.
18 Answer A.The T1W postcontrast MRI shows a mass with lobulated margins and continuous rim enhancement. The mass is only mildly T2 hyperintense, less than expected in a hemangioma or a fluid collection such as an abscess (not an answer choice). A smaller lesion is present anteriorly. The patient has a history of colon cancer, and these findings are compatible with metastatic disease. A simple cyst would have an imperceptible wall without enhancement and marked T2 hyperintensity. Focal nodular hyperplasia does not show rim enhancement and is most often found in premenopausal women.
Metastases can have a variety of appearances. The peripheral nodular tissue or progressive enhancement associated with some metastases should not be mistaken for a cavernous hemangioma. To make the diagnosis of a hemangioma based on its enhancement pattern, a discontinuous rim of nodularity should be identified during one of the phases of enhancement. In contradistinction, the rim enhancement associated with metastases is usually continuous. Metastases that have central necrosis or a cystic component can show increased signal on T2W images.
Hepatic metastases are the most common malignant liver lesion. Adenocarcinomas are the most common type of metastasis in the liver, most often from lung, colon, pancreas, breast, and stomach primaries. Most metastases including colorectal cancer metastases are T1 hypointense and somewhat T2 hyperintense. Most metastases are hypointense to liver on venous phase. If MRI is performed with hepatobiliary contrast agents, metastases are hypointense on 20-minute hepatobiliary phase as they lack normal functioning hepatocytes.
References: Namasivayam S, Martin DR, Saini S. Imaging of liver metastases: MRI. Cancer Imaging 2007;7:2–9.
Tirumani SH, Kim KW, Nishino M, et al. Update on the role of imaging in management of metastatic colorectal cancer. Radiographics 2014;34(7):1908–1928.
19a Answer B.There is marked diffuse loss of signal intensity in the liver and spleen on the in-phase relative to the out-of-phase images. Findings are consistent with hemosiderosis, a form of secondary hemochromatosis which occurs with repeated blood transfusions. In this condition, iron is deposited in the form of hemosiderin in the reticuloendothelial system including the liver and spleen.
In contradistinction, iron deposition in primary (hereditary) hemochromatosis spares the spleen. Major organs involved in primary hemochromatosis besides the liver include the pancreas and heart, organs not typically involved in hemosiderosis. Primary hemochromatosis is an autosomal recessive hereditary disorder associated with elevated intestinal absorption of iron. Iron deposition is toxic and leads to organ dysfunction and malignancy, including cirrhosis, hepatocellular carcinoma, diabetes, and cardiac dysfunction. “Bronze diabetes” refers to pancreatic dysfunction and skin hyperpigmentation in these patients. Other conditions such as cirrhosis can also lead to increased iron absorption and deposition sparing the spleen. Hemochromatosis is one of the causes of a hyperdense liver seen on noncontrast CT.
Techniques have been developed to quantify the degree of iron deposition with MRI sequences performed with progressively longer TE. Region of interest (ROI) values in the liver from each of the sequences can be used to estimate the iron concentration. Good correlation with hepatic biopsy specimens have been found with this technique. Quantification can provide information on the severity of the disease and effectiveness of treatment sparing repeated biopsies.
Treatment of primary hemochromatosis is repeated phlebotomy. Since patients with hemosiderosis have underlying anemia, phlebotomy is not advised. Iron chelation using drugs like deferoxamine is an option if treatment is felt to be necessary. Liver transplant can be considered in cases of primary hemochromatosis that progress to cirrhosis.
References: Chundru S, Kalb B, Arif-Tiwari H, et al. MRI of diffuse liver disease: the common and uncommon etiologies. Diagn Interv Radiol 2013;19(6):479–487.
Queiroz-Andrade M, Blasbalg R, Ortega CD, et al. MR imaging findings of iron overload. Radiographics 2009;29(6):1575–1589.
19b Answer C.T2* susceptibility effects would be diminished on spin-echo and short TE sequences compared to gradient-echo (GRE) and longer TE sequences. The T2* susceptibility effect of iron degrades the transverse magnetization vector that is needed to produce a signal. This effect actually results in signal loss on both T1W and T2W images. Since the T1W in-phase images are performed with a longer TE at 1.5 tesla (4.6 msec in-phase compared to 2.3 msec out-of-phase), the signal loss with iron is greater on in-phase images. This is the opposite of steatosis in which signal loss is greater on the out-of-phase images due to the intravoxel cancellation of the water- and fat-bound protons.
In the case of iron deposition as shown in the previous question, T2* effects can be helpful in diagnosis. However, these effects may produce susceptibility artifacts that degrade image quality. The heterogeneity of the magnetic field induced by susceptibility can result in image distortion and poor fat saturation in the area of interest. These effects are particularly noticeable with metals or at interfaces between two substances of significantly different susceptibilities. An interface that is prone to susceptibility effects is air with soft tissue (e.g., where lung bases meet the upper abdomen). Other than using fast spin-echo and short TE sequences, techniques to reduce susceptibility include increasing receiver bandwidth, increasing echo train length, and applying corrective reconstruction algorithms in some cases to restore spatial fidelity.
References: Mangrum WI, Merkle EM, Song AW. Chapter 8: Susceptibility artifact. In: Mangrum WI, Christianson KL, Duncan SM, et al. (eds). Duke review of MRI principles: case review series. Philadelphia, PA: Mosby, 2012:111–126.
Morelli JN, Runge VM, Ai F, et al. An image-based approach to understanding the physics of MR artifacts. Radiographics 2011;31(3):849–866.
20a Answer A.This small lesion is hypervascular, with enhancement in the arterial phase greater than surrounding liver. Enhancement is homogeneous and persists into the delayed phase, with signal intensity remaining greater than surrounding liver. This pattern of enhancement in conjunction with “light bulb” T2 hyperintensity is consistent with a capillary (“flash-filling”) hemangioma. Flash-filling hemangiomas are small, usually <2 cm. The enhancement pattern described is demonstrated on multiphase MR using conventional extracellular contrast agent and on CT. Hepatocellular carcinoma and metastases typically do not show enhancement greater than the liver on delayed imaging, and the pretest probability for liver metastasis in this patient is low with breast DCIS. Although focal nodular hyperplasia and hepatocellular adenoma have avid arterial enhancement, they tend to be nearly isointense to surrounding liver on precontrast T1 and T2 images as well as the postcontrast venous and delayed phases.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Silva AC, Evans JM, McCullough AE, et al. MR imaging of hypervascular liver masses: a review of current techniques. Radiographics 2009;29(2):385–402.
20b Answer C.The finding adjacent to the hemangioma represents a transient hepatic intensity difference (THID, which is analogous to a transient hepatic attenuation difference, or THAD, on CT). A THID or THAD is a wedge-shaped or geographic area of enhancement representing altered perfusion. It is often more apparent on one phase (usually arterial) than other phases. A THID can be seen around a rapidly-enhancing lesion such as this capillary hemangioma or other benign or malignant lesions. THIDs may also be associated with vascular abnormalities such as portal venous thrombosis. This THID is seen only on arterial phase. The other answer choices (hemorrhage, poor fat saturation, and focal fatty sparing) may appear hyperintense on T1W images but would be seen on the other postcontrast series as well.
References: Colagrande S, Centi N, Galdiero R, et al. Transient hepatic intensity differences. Part 1. Those associated with focal lesions. AJR Am J Roentgenol 2007;188(1):154–159.
Colagrande S, Centi N, Galdiero R, et al. Transient hepatic intensity differences. Part 2. Those not associated with focal lesions. AJR Am J Roentgenol 2007;188(1):160–166.
21 Answer A.The MRI demonstrates a mass in the right lobe with loss of signal on out-of-phase images compared to in-phase images in keeping with the presence of microscopic lipid. A portion of the mass enhances on the arterial phase, and there is washout and capsule appearance on delayed phase. In a patient with chronic hepatitis B, this is consistent with a hepatocellular carcinoma (HCC). A subset of HCCs accumulates microscopic or macroscopic fat. On MRI, fat-containing HCCs can be mildly hyperintense to the background liver on T1W images, as seen in the first image of this case.
Hepatocellular adenomas (HCAs) and angiomyolipomas (AMLs) may contain fat, but are not a consideration in this patient at risk for HCC. Angiomyolipoma (AML) is a benign mesenchymal tumor that is rarely found in the liver, and about half of the cases in the liver demonstrate macroscopic fat. Nodular steatosis is typically iso- to hypoenhancing on all postcontrast FS T1W series with no arterial-enhancing foci.
References: Choi JY, Lee JM, Sirlin CB. CT and MR imaging diagnosis and staging of hepatocellular carcinoma: Part I. Development, growth, and spread: key pathologic and imaging aspects. Radiology 2014;272(3):635–654.
Prasad SR, Wang H, Rosas H, et al. Fat-containing lesions of the liver: radiologic-pathologic correlation. Radiographics 2005;25(2):321–331.
22a Answer C.The contrast-enhanced CT in this patient with blunt trauma reveals linear and patchy areas of hypodensity representing hepatic and splenic lacerations. No intervention is needed if patient is hemodynamically stable. The liver laceration extends centrally toward the right hepatic vein and approaches the intrahepatic IVC without frank vascular disruption. Findings are most consistent with a grade IV laceration according to the most widely used liver injury grading scale, the American Association for the Surgery of Trauma (AAST) classification.
AAST Classification of Liver Injury
*Advance one grade for multiple injuries up to grade III.
Despite the extent of the laceration on CT, surgery is generally reserved for those who are hemodynamically unstable. Not all the features on the scale can be accurately assessed with imaging (CT tends to underestimate grade), but the scale allows estimation of likelihood of success with nonoperative management. About 70% to 90% of cases are now managed nonoperatively with 90% success rate. Hepatic avulsion (grade VI) is the only grade that absolutely requires surgery, since patients are invariably hemodynamically unstable. There is a higher likelihood of success for nonoperative management with lower grade (I to III) injuries than with higher grade (IV to V) injuries. Regarding the other answer choices, there is no evidence of active arterial hemorrhage or pseudoaneurysm to embolize. No subcapsular hematoma is seen and, even if present, would not require percutaneous drainage in uncomplicated cases.
References: Poletti PA, Mirvis SE, Shanmuganathan K, et al. CT criteria for management of blunt liver trauma: correlation with angiographic and surgical findings. Radiology 2000;216(2):418–427.
Yoon W, Jeong YY, Kim JK, et al. CT in blunt liver trauma. Radiographics 2005;25:87–104.
22b Answer A.The HIDA scan shows contrast uptake by the liver and excretion into the bile ducts, gallbladder, and small bowel. Two foci of intrahepatic bile accumulation superior and lateral to the gallbladder are compatible with bilomas (arrows), which were confirmed at ERCP.
Bilomas in liver laceration.
With hepatic injury being managed nonoperatively, the development of bilomas is fairly common, seen in up to 20% of patients. Patients may complain of increased abdominal pain or have jaundice, fever, and leukocytosis. CT may show low-density fluid collections or ascites. Bile leaks are generally managed nonoperatively with ERCP and stenting, but percutaneous drainage or laparotomy may be indicated for superinfection of a biloma or for bile peritonitis.
References: Gupta A, Stuhlfaut JW, Fleming KW, et al. Blunt trauma of the pancreas and biliary tract: a multimodality imaging approach to diagnosis. Radiographics 2004;24:1381–1395.
Mettler FA, Guiberteau MJ. Chapter 7: Gastrointestinal tract. In: Mettler FA, Guiberteau MJ (eds). Essentials of nuclear medicine imaging, 6th ed. Philadelphia, PA: Elsevier/Saunders, 2012:237–270.
23 Answer D.The main portal vein is not seen. In its place, numerous tortuous periportal collateral vessels are consistent with “cavernous transformation of the portal vein” in the setting of chronic portal vein occlusion. This collateralization can take about a year to develop and is therefore typically associated with benign disease. This patient had a history of portal vein thrombosis as a result of prior pancreatitis. On ultrasound, tortuous anechoic veins can be seen, which demonstrate low-level hepatopedal venous waveform consistent with portal-type flow. In addition to varices, other findings of portal hypertension that may be seen include splenomegaly and ascites.
Varices represent portosystemic collateral pathways in the setting of portal hypertension. These may drain into the superior vena cava and/or the inferior vena cava. The following images are from a patient with cirrhosis and portal hypertension showing extensive varices. The left gastric, or coronary, vein (black arrow) is seen arising from the portal vein and represents a commonly recognized varix. It travels in the gastrohepatic ligament, communicating with esophageal and paraesophageal varices as demonstrated on the second image. These varices drain into the SVC. The third CT image shows “recanalization of the umbilical vein” (white arrow) in the fissure for the falciform ligament. The coronary, short gastric, and splenic veins communicate with the left renal vein, allowing for gastrorenal and splenorenal shunts in portal hypertension. These shunts ultimately drain into the IVC.
Varices in portal hypertension, including the coronary vein (black arrow), esophageal varices, and recanalized umbilical vein (white arrow).
Portal hypertension may be classified as presinusoidal, sinusoidal (intrahepatic), or postsinusoidal. Common causes are listed in the table below.
Common Causes of Portal Hypertension
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Morgan T, Qayyum A. Chapter 89: Diffuse liver disease. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1629–1675.
24a Answer B.This arterial-enhancing mass is isodense on the precontrast and venous and delayed postcontrast images, so closely matching the surrounding liver parenchyma that it is imperceptible. This appearance may be a clue (especially when taking into account the patient’s age, sex, and clinical scenario) that the mass is of hepatocellular origin—either a focal nodular hyperplasia (FNH) or hepatocellular adenoma (HCA). (In a young woman without chronic liver disease HCC is unlikely.) HCA was the diagnosis at biopsy.
HCAs are now believed to represent a heterogeneous group of tumors of hepatocellular origin. HCAs occasionally have microscopic lipid and do not typically exhibit a central scar. Because hepatic adenomas lack functioning bile ducts, they will transition from arterial enhancement to hypointensity on hepatobiliary phase when a hepatobiliary contrast agent such as Eovist is used. Hepatobiliary phase MRI is highly sensitive and specific for distinguishing HCA and FNH, as FNH retains contrast.
Regarding the other answer choices, isodensity on the venous or delayed phases is not “washout”. To meet criteria for “washout” this hypervascular mass should subsequently appear hypodense to the surrounding liver. In addition, washout appearance outside of the patient population with chronic liver disease is not specific for HCC and may not indicate malignancy. LI-RADS categorization is not appropriate in this case because this patient is not at risk for HCC. THADs are areas of altered perfusion in otherwise normal parenchyma that can be arterial enhancing and imperceptible on other pre- and postcontrast series. A THAD of this size should appear more geographic, not round and mass-like. THADs are associated with an underlying cause such as an adjacent mass, portal vein thrombosis, or cirrhosis. Hypervascular metastases may have a similar enhancement pattern to HCA in which small subtle metastases are only detectable on arterial phase images. However, metastases of this size tend to appear more distinct from surrounding liver on pre- and postcontrast CT and MR images. Hypervascular metastases would be less likely than FNH or HCA in a young patient without known history of malignancy.
References: Grazioli L, Bondioni MP, Haradome H, et al. Hepatocellular adenoma and focal nodular hyperplasia: value of gadoxetic acid-enhanced MR imaging in differential diagnosis. Radiology 2012;262(2):520–529.
Katabathina VS, Menias CO, Shanbhogue AK, et al. Genetics and imaging of hepatocellular adenomas: 2011 update. Radiographics 2011;31(6):1529–1543.
24b Answer B.Among the answer choices, men are at greater risk for malignant transformation of hepatocellular adenomas (HCAs). Three subtypes of HCA have been described with different genetics and thought to represent separate entities, with a fourth category for tumors that are unable to be classified. Overall, risk of hemorrhage and rupture is 20% to 25%, and risk of malignant transformation to HCC is 5% to 10%. Imaging has an important role in monitoring for growth and guiding biopsy. There may be some imaging features suggestive of a subtype, but imaging currently does not reliably distinguish among the subtypes. Of particular concern is the β-catenin–mutated type which is associated with the highest risk of malignant transformation to HCC, and is not associated with a specific imaging pattern. This type occurs more commonly in men. Other risk factors for β-catenin–mutated type are listed in the following table. Biopsy may be indicated for risk stratification and to exclude hypervascular metastases if there is a concern for malignancy.
Subtypes of Hepatocellular Adenomas
Initial management of HCAs involves withdrawal of oral contraceptives or steroids. Closer monitoring or intervention (embolization or surgical resection) may be considered for tumors >5 cm, men, patients with glycogen storage disease, and β-catenin–mutated type as these are risk factors for complications. Patients who arbitrarily have >10 tumors in number are designated as having adenomatosis, which can apply to any subtype. Risk for rupture and malignancy depend on the characteristics of the underlying subtype.
References: Grazioli L, Bondioni MP, Haradome H, et al. Hepatocellular adenoma and focal nodular hyperplasia: value of gadoxetic acid-enhanced MR imaging in differential diagnosis. Radiology 2012;262(2):520–529.
Katabathina VS, Menias CO, Shanbhogue AK, et al. Genetics and imaging of hepatocellular adenomas: 2011 update. Radiographics 2011;31(6):1529–1543.
25a Answer D.Fibrolamellar hepatocellular carcinoma (FHCC) is the option among the choices listed that best fits the imaging pattern. This mass shows features that have been associated with FHCC. The large mass shows a central scar, which is found in the majority of FHCCs. There is heterogeneous arterial enhancement. The lesion is hypointense on the 20-minute hepatobiliary phase. Small satellite nodules are noted in the left lobe. About half of the patients show regional nodal spread at presentation.
Top differential diagnoses in a young woman with a hypervascular mass are focal nodular hyperplasia (FNH) and hepatocellular adenoma (HCA). The mass in this case has morphology resembling FNH with lobulated margins, arterial enhancement, and central scar, but nearly all FNHs retain contrast on hepatobiliary phase, while FHCCs appear hypointense as shown here. Appearance of FHCC on CT or MRI performed with a conventional extracellular contrast agent is more variable in the venous and delayed phases, ranging from hypo- to hyperintense.
Regarding the other answer choices, colon carcinoma metastases are typically hypovascular without significant arterial enhancement. Although giant cavernous hemangiomas can be hypointense on hepatobiliary phase and contain a central scar, there is no peripheral nodular discontinuous enhancement or “light bulb” T2 hyperintensity to indicate hemangioma. HCAs and hypervascular metastases are not listed among the answer choices, but they can also show arterial enhancement with hypointensity on hepatobiliary phase. However, they do not typically show a central scar.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Ganeshan D, Szklaruk J, Kundra V, et al. Imaging features of fibrolamellar hepatocellular carcinoma. AJR Am J Roentgenol 2014;202(3):544–552.
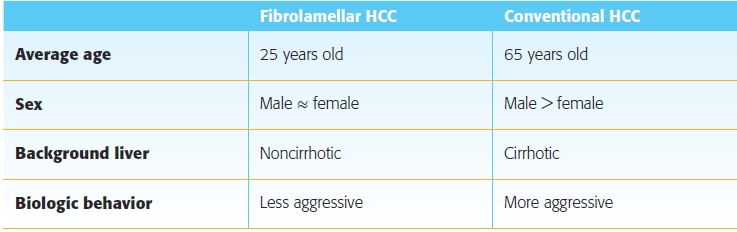
25b Answer A.Fibrolamellar hepatocellular carcinoma (FHCC) is a rare malignancy that accounts for fewer than 1% of hepatocellular carcinomas. There is unimodal distribution with about 85% of patients younger than 40 years of age, whereas fewer than 5% of patients with conventional hepatocellular carcinoma (HCC) are younger than 40 years. Focal nodular hyperplasia (FNH) and hepatocellular adenoma (HCA) are more common in women, but there is no sex predilection in FHCC. FNH, HCA and FHCC occur in noncirrhotic livers, whereas conventional HCC most often develops in the setting of cirrhosis. FHCC tumorigenesis is thought to be distinct from that of HCC. Serum α-fetoprotein levels are normal. Tumors are frequently large at discovery with nonspecific symptoms due to size. There is evidence that the tumor is less aggressive than conventional HCC, with higher overall 5-year survival of 40% compared to about 7% for conventional HCC. The following table summarizes important demographic and clinical distinctions between FHCC and conventional HCC.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Ganeshan D, Szklaruk J, Kundra V, et al. Imaging features of fibrolamellar hepatocellular carcinoma. AJR Am J Roentgenol 2014;202(3):544–552.
26 Answer D.The most common benign tumor found in the liver is hemangioma. It is thought to have a prevalence of up to 20% of the population based on autopsy series. The tumor could be considered a hamartomatous proliferation of endothelium rather than a true neoplasm. Hemangiomas are usually asymptomatic and incidentally noted. Focal nodular hyperplasia (FNH) is the second most common and hepatocellular adenoma (HCA) the third most common benign liver tumor. Metastases are overall the most common malignant tumor found in the liver. Hepatocellular carcinoma (HCC) is the most common primary liver malignancy.
Hemangioma, FNH, HCA, and HCC are hypervascular (i.e., arterial enhancing). A summary of benign and malignant hypervascular masses with key features is presented in the following chart. When evaluating a hypervascular tumor, the first step is to determine if it is a benign hemangioma that requires no further follow-up or intervention.
Abbreviation of MRI contrast type: EC, extracellular; and HB, hepatobiliary.
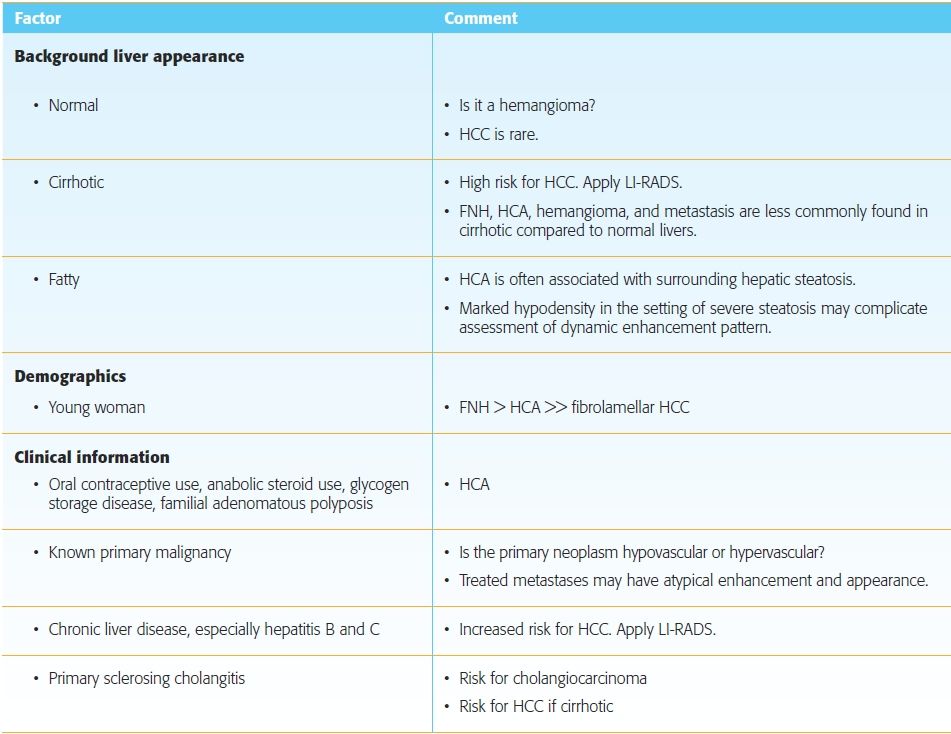
Patient demographics, clinical information, and background liver appearance are also important in the assessment of hypervascular liver tumors. Pointers for incorporating this information into the interpretation of imaging findings are summarized in the following table.
Important Considerations in the Assessment of Hypervascular Liver Tumors
References: Grand DJ, Mayo-Smith WW, Woodfield CA. Practical body MRI: protocols, applications, and image interpretation. Cambridge, UK: Cambridge University Press, 2012.
Khosa F, Khan AN, Eisenberg RL. Hypervascular liver lesions on MRI. AJR Am J Roentgenol 2011;197(2):W204–W220.
Silva AC, Evans JM, McCullough AE, et al. MR imaging of hypervascular liver masses: a review of current techniques. Radiographics 2009;29(2):385–402.
27 Answer A.This case demonstrates the sequela of passive hepatic congestion. With congestive heart failure (and other causes of increased right heart pressures such as constrictive pericarditis and pericardial effusion), elevated pressures are transmitted retrograde into the IVC and hepatic veins. These vessels become engorged, and venous return to the heart is impaired resulting in passive congestion of the liver. Reflux of contrast from the heart into the IVC may be demonstrated on early phases of enhancement. The parenchyma may demonstrate a diffusely mottled appearance with curvilinear hypodensities, referred to as “nutmeg liver,” which is also evident on the following image from a different patient with extensive history of cardiac surgery. In early or acute disease, the liver is enlarged. Treatment is aimed at controlling the underlying cardiac disease to prevent cirrhosis.
Nutmeg liver.
Regarding the other answer choices, heterogeneity of the liver in Budd-Chiari syndrome is accompanied by thrombosis or attenuation of the IVC and hepatic veins, not enlargement. An enlarged IVC may be seen due to the abnormal venous drainage from an arteriovenous malformation (AVM), however, enlarged tortuous hepatic arterial branches should be identified. Hepatic infarcts are peripheral and wedge-shaped areas of decreased enhancement. Hepatic infarcts are uncommon given the dual vascular supply of the liver, but compromise of both the hepatic arterial and portal venous supply can occur in trauma, after interventions such as surgery and chemoembolization, in liver transplantation or with hypercoagulable states.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Torabi M, Hosseinzadeh K, Federle MP. CT of nonneoplastic hepatic vascular and perfusion disorders. Radiographics 2008;28(7):1967–1982.
28 Answer C.The foci of restricted diffusion on apparent diffusion coefficient (ADC) map in this mass correspond to nonenhancing T2 bright loculations of fluid in this hepatic abscess. This is secondary to restriction of water molecules in densely packed, thick pyogenic material. The FS T1W postcontrast image shows the classic “cluster-of-grapes” appearance compatible with abscess, representing small areas of liquefying liver parenchyma. Restricted diffusion is seen in abscesses as well as some tumors. Neoplasms may have restricted diffusion due to hypercellularity. However, patients with neoplasms that have necrosis or cystic changes tend to have increased diffusion in the liquid portions. Gas and iron are expected to be dark on all series.
There is substantial overlap in the appearance of benign and malignant lesions on diffusion-weighted imaging, so images must be interpreted in conjunction with other imaging features and the clinical scenario. Restricted diffusion is bright on diffusion series and dark on ADC map. Restricted diffusion has been reported in metastases, hepatocellular carcinoma, adenoma, focal nodular hyperplasia, abscess, and hematoma. Diffusion series may improve detection of number of lesions if lesions are bright and surrounding anatomy is suppressed, as b values increase. Hemangiomas and other markedly T2 hyperintense lesions may show T2 shine-through rather than true diffusion restriction correlating with brightness on ADC map. Diffusion series are prone to distortion and degradation by susceptibility artifact.
References: Kanematsu M, Goshima S, Watanabe H, et al. Detection and characterization of focal hepatic lesions with diffusion-weighted MR imaging: a pictorial review. Abdom Imaging 2013;38(2):297–308.
Lee NK, Kim S, Kim DU, et al. Diffusion-weighted magnetic resonance imaging for non-neoplastic conditions in the hepatobiliary and pancreatic regions: pearls and potential pitfalls in imaging interpretation. Abdom Imaging 2015;40(3):643–662.
29 Answer D.This constellation of findings is consistent with a cholangiocarcinoma (CCA). Multiple dilated biliary ducts in the left lobe converge on a mass that is mildly hypointense on T1W and mildly hyperintense on T2W images. The mass remains hypointense on arterial phase and then shows progressive enhancement on the delayed phase typical of the fibrosis within the tumor. As in this case, enhancement is often ill-defined and blends in with the surrounding liver such that the lesion may be better appreciated on the precontrast rather than postcontrast images. Although the enhancement appears to “fill in” on delayed phase, this mass has neither the discontinuous peripheral nodular enhancement nor the “light bulb” T2 hyperintensity expected of a hemangioma. If a hepatobiliary contrast agent such as Eovist is used, CCAs would be hypointense on the 20-minute hepatobiliary phase as expected for any mass without functioning hepatocytes.
Even small CCAs can cause biliary ductal obstruction with lobar atrophy and capsular retraction. The parenchymal atrophy is a result of underlying biliary obstruction and/or portal vein occlusion. These findings may be accompanied by surrounding geographic regions of altered enhancement, as seen in this case. Areas of hepatic atrophy and biliary dilation must be carefully inspected for an underlying cause such as CCA and not assumed to be from a past benign insult. Ascending (acute bacterial) cholangitis may be more likely to develop in patients with various causes of biliary obstruction but is not the best answer choice because the key finding in this case is a malignant mass. On occasion, tumors such as large intrahepatic metastases (not among the answer choices) can cause biliary obstruction. No hypervascularity on arterial phase or washout appearance on subsequent phases is seen to suggest hepatocellular carcinoma (not among the answer choices), although CCAs can occasionally show patchy areas of arterial enhancement. HCCs do not progressively enhance.
References: Chung YE, Kim MJ, Park YN, et al. Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics 2009;29(3):683–700.
Sainani NI, Catalano OA, Holalkere NS, et al. Cholangiocarcinoma: current and novel imaging techniques. Radiographics 2008;28(5):1263–1287.
30 Answer A.Linear branching hypodensities associated with surrounding wedge-shaped–altered enhancement in the anterior segment right lobe are most consistent with intrahepatic portal vein thrombosis (PVT). Areas of parenchymal perfusional abnormality representing transient hepatic attenuation/intensity differences (THADs on CT and THIDs on MRI) should be closely examined for PVT, arterioportal shunts, and masses.
The dynamics of the liver’s dual blood supply account for the THADs/THIDs seen with PVT. The affected region receives increased hepatic arterial inflow to compensate for the decreased portal venous inflow, accounting for the increased regional density in the early phases of enhancement. The perfusional differences are transient or become less evident on later phases as the unaffected liver progressively enhances. This patient had bland thrombus, which may be associated with cirrhosis, inflammation, hypercoagulable states, and percutaneous hepatobiliary procedures. PVT may also be due to tumor invasion, most commonly hepatocellular carcinoma in cases of intrahepatic thrombus, and pancreatic or gastric carcinoma if extrahepatic. Half of patients with PVT have no identifiable cause. Thrombus enhancement is consistent with tumor thrombus but may be difficult to detect reliably with any imaging modality. Significant vein expansion tends to favor tumor over bland thrombus. Patients with acute PVT may be treated with anticoagulation and correction of underlying cause.
Regarding the other answer choices, liver laceration extending to the vessels may be a cause of PVT, but the overlying parenchyma is intact. Branching hypodensity can also be seen with biliary ductal dilation, but in this case, the hypodensity follows the expected course of the portal veins indicating thrombus. Fatty sparing can be seen as geographic areas of normal density, but in this case, the geographic density is a THAD reflecting altered perfusion around the thrombus.
References: Gore RM, Ba-Ssalamah A. Chapter 90: Vascular disorders of the liver and splanchnic circulation. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1676–1705.
Lee WK, Chang SD, Duddalwar VA, et al. Imaging assessment of congenital and acquired abnormalities of the portal venous system. Radiographics 2011;31(4):905–926.
31 Answer B.A circumscribed focus of enhancement (arrows) is seen in the porta hepatis that follows the aorta on all phases. It is surrounded by hematoma, and there is no contrast dispersal. This arises from a branch of the proper hepatic artery adjacent to a surgical clip, best demonstrated on the coronal arterial image. Findings are consistent with a hepatic artery pseudoaneurysm. Contrast dispersal would indicate active extravasation rather than pseudoaneurysm.
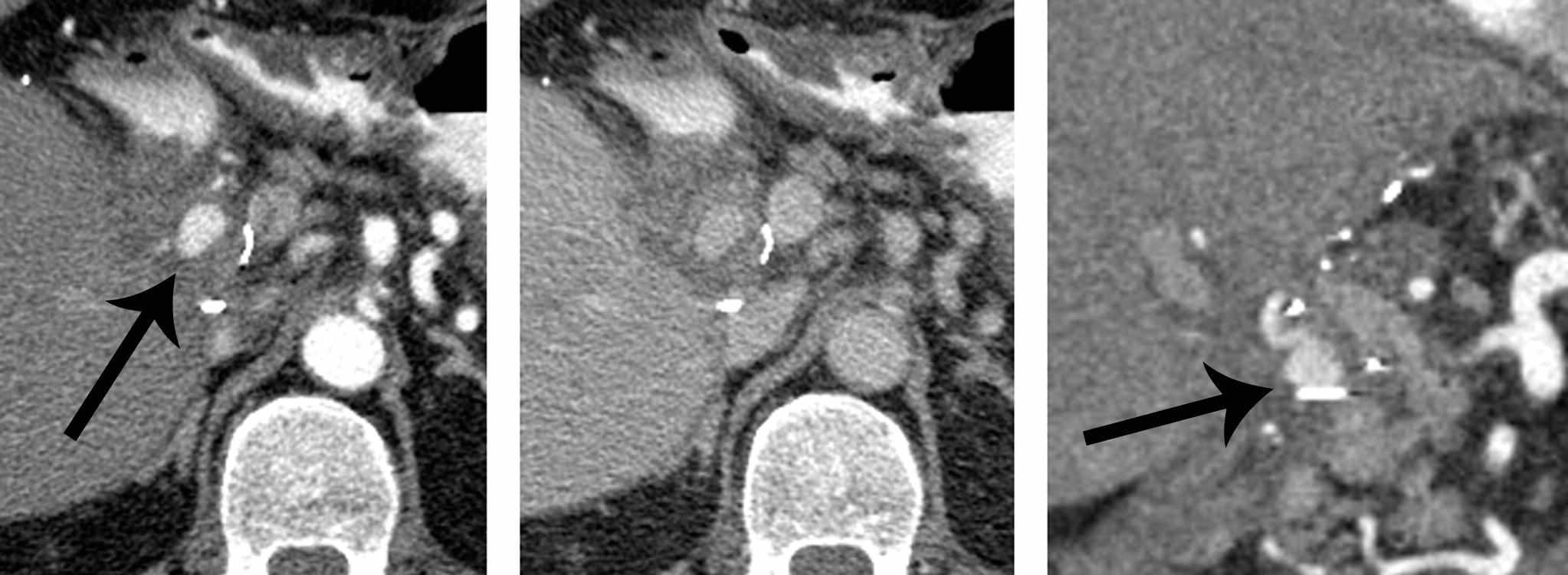
Hepatic artery aneurysms are the second most common visceral artery aneurysm accounting for 20% of cases overall, after splenic artery aneurysms (60%). Most hepatic artery aneurysms are symptomatic, and patients can present with hemorrhage into the gastrointestinal tract or surgical drains, followed by jaundice. Extrahepatic aneurysms are often degenerative and more common than intrahepatic aneurysms. Intrahepatic aneurysms are due to other causes including trauma, biopsy, other surgical/interventional procedures, infection, or vasculitis. There is a high incidence of rupture, which is a catastrophic event with >80% mortality. Urgent interventional radiology consultation for embolization is the most appropriate next step. The following image from the selective hepatic artery arteriogram in this patient confirmed the pseudoaneurysm, and embolization was performed.
Hepatic artery pseudoaneurysm.
References: Gore RM, Ba-Ssalamah A. Chapter 90: Vascular disorders of the liver and splanchnic circulation. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1676–1705.
Jesinger RA, Thoreson AA, Lamba R. Abdominal and pelvic aneurysms and pseudoaneurysms: imaging review with clinical, radiologic, and treatment correlation. Radiographics 2013;33(3):E71–E96.
32 Answer B.Ultrasound of the liver shows a “starry-sky” appearance. Diffuse edema causes the appearance of decreased echogenicity of the liver parenchyma. The walls of the portal venules become more conspicuous and represent the “stars” against the night “sky” of the edematous parenchyma. The most common cause of “starry-sky” appearance is acute hepatitis. In this patient, acute alcoholic hepatitis was thought to be the cause. However, “starry-sky” appearance has also been described with other processes that cause liver edema or infiltration, such as toxic shock, right heart failure, leukemia, and lymphoma.
The diagnosis of acute hepatitis is usually based on clinical history, liver function tests (LFTs), and serologic tests. Imaging such as ultrasound is useful to evaluate for alternate diagnoses such as biliary pathology that may require intervention. Treatment of patients with acute hepatitis is supportive, with mild-to-moderate cases manageable on an outpatient basis. Severe or fulminant cases of acute hepatitis may require intensive hospital care.
References: Abu-Judeh HH. The “starry sky” liver with right-sided heart failure. AJR Am J Roentgenol 2002;178(1):78.
Morgan T, Qayyum A, Gore RM. Chapter 89: Vascular disorders of the liver and splanchnic circulation. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1629–1675.
33a Answer C.There is a mass with internal hemorrhage in a background of hepatic steatosis. The first two MR images are T1W in-phase and out-of-phase images showing diffuse drop in signal intensity on out-of-phase images of the background liver parenchyma compatible with hepatic steatosis. In hemosiderosis, the liver would drop in signal intensity on the in-phase images due to increased magnetic susceptibility on longer TE images. The liver mass contains a small focus of T1 hyperintensity that persists on the fat-saturated T1W image, indicating hemorrhage rather than macroscopic fat.
33b Answer B.
In a young woman with a hemorrhagic liver mass in a background of hepatic steatosis, the most likely diagnosis is hepatocellular adenoma (HCA). While focal nodular hyperplasia (FNH) is more common than HCA, FNH does not have propensity to hemorrhage and rupture. In light of the patient’s age and absence of risk factors for hepatocellular carcinoma (HCC) or primary malignancy, HCC and metastatic disease are unlikely.
HCAs are most commonly found in women of childbearing age taking oral contraceptives, but as discussed in a previous question, they also develop in patients with glycogen storage disease and those taking exogenous androgens. HCAs can be heterogeneous due to intralesional fat or hemorrhage. Intervention including embolization or surgical resection could be considered in lesions >5 cm or those with hemorrhage.
References: Fisher A, Siegelman ES. MR techniques and MR of the liver. In: Siegelman ES (ed). Body MRI. Philadelphia, PA: Elsevier Saunders, 2005:4–5.
Katabathina VS, Menias CO, Shanbhogue AK, et al. Genetics and imaging of hepatocellular adenomas: 2011 update. Radiographics 2011;31(6):1529–1543.
34 Answer C.Noncontrast image of the liver shows crescentic high attenuation conforming to the margins of the lateral segment left lobe of the liver. This is consistent with a subcapsular hematoma in this patient who had a percutaneous liver biopsy earlier in the day. The sudden pain is attributed to acute distention of the Glisson capsule of the liver. CT is the study of choice for evaluation of suspected hemorrhage. The density of an acute hematoma (1 to 3 days) decreases as the hematoma evolves, and a pseudocapsule may develop in 2 to 4 weeks. Mixed density can be seen with layering clot (hematocrit effect) or hemorrhage of different ages. Subcapsular hematomas are typically crescentic or biconvex (lenticular) in shape. Management of hemorrhage may include blood transfusion and transcatheter arterial embolization if clinically warranted. This patient was stable and treated conservatively without intervention.
This patient does have diffuse hepatic steatosis, accounting for diffuse low density of the liver, which makes the unenhanced vessels visible on this noncontrast exam, but the crescentic subcapsular configuration of the high-density area is not typical for fatty sparing. Transient hepatic attenuation difference (THAD) refers to altered parenchymal enhancement that tends to disappear on later phases and would not be applicable to this noncontrast exam. Periportal edema may be seen with trauma, acute hepatitis, and congestion and manifests as a halo of low density around the portal triads, not seen here.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Casillas VJ, Amendola MA, Gascue A, et al. Imaging of nontraumatic hemorrhagic hepatic lesions. Radiographics 2000;20(2):367–378.
35 Answer A.The arterial phase on the current study is too early, limiting evaluation for hypervascular neoplasms. Images in a liver protocol MRI or CT should be acquired in the late arterial phase, when there is a heterogeneous blush of contrast in the main portal vein (long arrow) as seen on the prior MRI exam. The current exam shows no contrast in the main portal vein (short arrow).
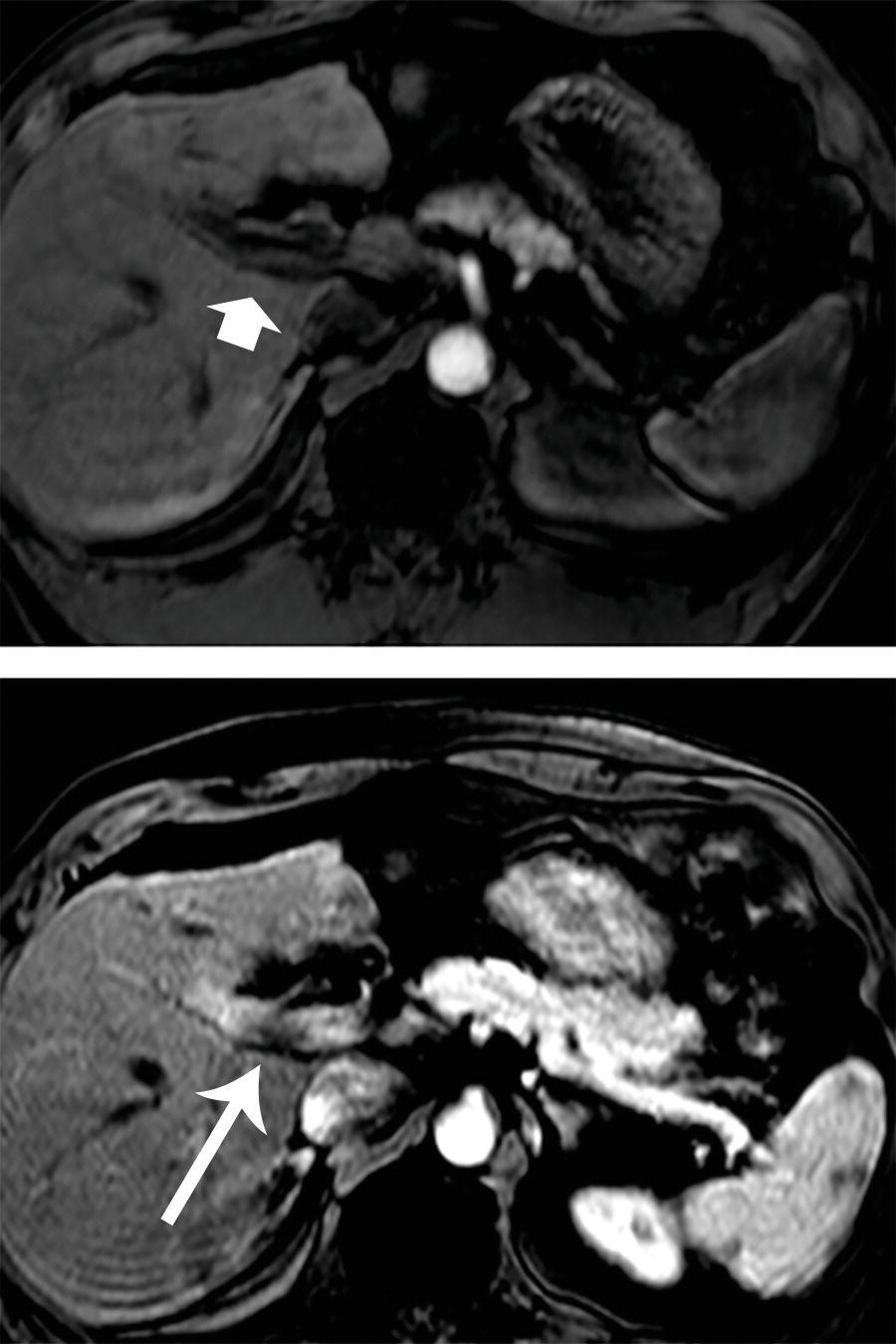
In the late arterial phase, sinusoidal enhancement of the spleen and corticomedullary phase enhancement of the kidneys are expected. However, on the current MRI in the top row, there is no contrast in the portal vein and no organ enhancement. (The pancreas has inherent T1 hyperintensity and normally appears brighter than other organs on an unenhanced T1 image.) A subsequent MRI 6 weeks later (not shown) revealed that the lesion was still present and slightly increased in size. The lesion was considered to be a hepatocellular carcinoma and treated with radiofrequency ablation.
Spontaneous regression or resolution of hypervascular nodules in the cirrhotic liver has been reported but is very rare, postulated to be due to interruption of arterial blood supply to small presumed dysplastic nodules or even HCCs. There is no vessel in line with the liver finding in the right lobe that would account for ghosting. Small benign arterial portal shunts (not an answer choice) are typically tiny hypervascular foci commonly seen in the cirrhotic liver and may account for transient hepatic intensity differences (THIDs). These may seem to appear and disappear from study to study, perhaps due to slight differences in bolus timing.
References: Boll DT, Merkle EM. Diffuse liver disease: strategies for hepatic CT and MR imaging. Radiographics 2009;29(6):1591–1614.
Gandhi SN, Brown MA, Wong JG, et al. MR contrast agents for liver imaging: what, when, how. Radiographics 2006;26(6):1621–1636.
36 Answer F.This patient has metastatic mucinous colorectal carcinoma. The liver is enlarged by confluent hypodense masses representing mucinous metastases. The density of the mucin is similar to but slightly greater than expected for simple fluid (with simple fluid up to about 20 HU). There is little evidence of soft tissue, and the appearance can be mistaken for a group of benign cysts such as in polycystic liver disease. In this case, there are other findings consistent with a malignant process including low-density metastatic lymphadenopathy that encases and narrows the portal vein best seen on the coronal image, as well as peritoneal carcinomatosis. At pathology, a tumor is defined as mucinous when >50% of the tumor is composed of mucin. Mucinous hepatic metastases are most frequently from colorectal carcinoma (CRC), with 10% to 20% of colorectal carcinomas meeting criteria. Calcification is more frequently seen in mucinous compared to nonmucinous CRC. Other mucinous primaries are less common than CRC but may be from the breast, ovary, pancreas, or other sites in the gastrointestinal tract.
Metastases can also appear cystic because of necrosis, with variable amounts of soft tissue visible internally. Necrosis can occur when tumor growth outstrips the vascular supply such as after treatment with locoregional therapies like ablation or systemic chemotherapy. The differential diagnosis of a multilocular cystic lesion may include biliary cystadenoma/cystadenocarcinoma and various infections in the appropriate clinical setting.
References: Ko EY, Ha HK, Kim AY, et al. CT differentiation of mucinous and nonmucinous colorectal carcinoma. AJR Am J Roentgenol 2007;188(3):785–791.
Qian LJ, Zhu J, Zhuang ZG, et al. Spectrum of multilocular cystic hepatic lesions: CT and MR imaging findings with pathologic correlation. Radiographics 2013;33(5):1419–1433.
37 Answer B.This patient has neuroendocrine tumor metastases. There are multiple small masses with arterial enhancement, indicating a hypervascular neoplasm. These metastases appear isodense to liver on delayed phases. Among the choices given, neuroendocrine tumors are hypervascular. (A small subset of breast metastases is hypervascular, but this patient is male, which makes the diagnosis much less likely.) Note that small cell lung cancer (SCLC) is considered a neuroendocrine neoplasm and may show hypervascular metastases, but SCLC is not an answer choice. Non-small cell lung cancer is among the answer choices but is not hypervascular.
The hypervascular neoplasms in the mnemonic “MR CT” are Melanoma, Renal cell carcinoma, Carcinoid (i.e., neuroendocrine tumor) or Choriocarcinoma, and Thyroid carcinoma. This patient had a Whipple procedure to resect a pancreatic neuroendocrine tumor. In contradistinction, pancreatic ductal adenocarcinoma is a hypovascular neoplasm without arterial enhancement. On the delayed phase, hypervascular metastases are typically iso- to hypodense when compared to the surrounding liver. Metastases do not typically show delayed enhancement like hemangiomas do. Keep in mind that metastases have a wide range of appearances, and findings should always be interpreted in light of the pathology of the underlying malignancy, appearance of the background liver, and treatment received.
References: Khosa F, Khan AN, Eisenberg RL. Hypervascular liver lesions on MRI. AJR Am J Roentgenol 2011;197(2):W204–W220.
Silva AC, Evans JM, McCullough AE, et al. MR imaging of hypervascular liver masses: a review of current techniques. Radiographics 2009;29(2):385–402.
38 Answer E.This patient with a liver transplant has a lymphoid tumor consistent with posttransplant lymphoproliferative disorder (PTLD). Biopsy revealed a lymphoma. The imaging findings in this case are nonspecific, with a hypoattenuating lesion on the arterial and venous phase CT and a “bull’s-eye” appearance on ultrasound. The differential diagnosis in this patient mainly includes abscess, PTLD, and recurrent hepatocellular carcinoma (HCC) with an atypical hypovascular appearance. Among the choices listed for this question, lymphoid tumor (PTLD) is the most likely diagnosis.
PTLD is a heterogeneous group of disorders ranging from benign hyperplasia to poor-differentiated lymphoma, but most lesions are monoclonal. The majority of cases are B-cell proliferations thought to be induced by Epstein-Barr virus (EBV). The liver is the most commonly involved organ in the abdomen, followed by small bowel and kidneys. PTLD in the liver most often presents as solitary or multiple masses with low attenuation on CT best seen on venous phase. Other manifestations of PTLD and lymphoid tumors are ill-defined infiltration of the parenchyma and periportal masses. Lymphoid tumors may encase periportal vessels without narrowing them, a feature that has been described as the “vessel penetration” sign. On ultrasound, lymphoid masses are typically hypoechoic, although lesions can be nearly anechoic or have a “bull’s-eye” appearance with a hyperechoic center and hypoechoic rim, as seen in this patient. Because imaging features overlap with opportunistic infections and other neoplasms in this immunosuppressed patient population, biopsy is usually required to make the diagnosis.
In adult transplant patients, PTLD is overall the second most common tumor (after nonmelanoma skin cancer). It is most often diagnosed within 1 year of transplant but can occur at any time. Treatment includes reduction in immunosuppression, with chemotherapy and radiation for frankly malignant tumors and refractory cases.
References: Borhani AA, Hosseinzadeh K, Almusa O, et al. Imaging of posttransplantation lymphoproliferative disorder after solid organ transplantation. Radiographics 2009;29(4):981–1000; discussion 1000–1002.
Camacho JC, Moreno CC, Harri PA, et al. Posttransplantation lymphoproliferative disease: proposed imaging classification. Radiographics 2014;34(7):2025–2038.
39 Answer D.This woman has breast cancer with widespread liver and splenic metastases. Pseudocirrhosis has developed after treatment with hepatic atrophy and lobulated contour. Pseudocirrhosis is a form of posttreatment sequela after chemotherapy for liver metastases. This condition has a predilection for breast cancer metastases for uncertain reasons and is uncommonly seen with other primary tumors. The liver contour can be finely or coarsely nodular, with areas of capsular retraction. The caudate lobe may also enlarge, as seen in some cases of cirrhosis. In some cases, nodular regenerative hyperplasia (NRH) with atrophy of intervening parenchyma without fibrosis has been found. In other cases, there is a desmoplastic response incited by an extensively infiltrating breast cancer. Although the true histopathologic findings of cirrhosis are not found in pseudocirrhosis, some patients nevertheless develop portal hypertension with varices and ascites. Other changes that can be found after treatment of liver metastasis include altered enhancement patterns, cystic/necrotic degeneration, and calcification.
References: Faria SC, Ganesan K, Mwangi I, et al. MR imaging of liver fibrosis: current state of the art. Radiographics 2009;29(6):1615–1635.
Jha P, Poder L, Wang ZJ, et al. Radiologic mimics of cirrhosis. AJR Am J Roentgenol 2010;194(4):993–999.
40 Answer C.This patient has the CT equivalent of the “hot spot sign” (originally described in Tc-99m sulfur colloid scans) which is diagnostic for superior vena cava (SVC) obstruction. SVC obstruction is due to lung cancer in up to 75% of cases, with non-small cell carcinoma accounting for most of those cases. Classically, there is intense early enhancement of the medial segment left hepatic lobe without underlying liver mass. This is associated with an extensive network of veins in the chest wall, mediastinum, and around the liver. These vessels form caval-to-portal collateral pathways in the setting of chronic SVC obstruction and are well depicted on CT and MRI. This could be considered a transient hepatic attenuation difference (THAD) due to altered perfusion. It usually has geographic margins and a pathognomonic appearance but could be mistaken for a hypervascular mass.
Catheter-related thrombosis is an increasing cause of SVC obstruction and may account for 15% to 40% of cases. Lymphoma as a cause of SVC obstruction accounts for 10% of cases. SVC obstruction may cause shortness of breath and redness and swelling of the face, neck, upper extremities, and chest wall. Management includes treating the underlying malignancy with chemotherapy and radiation, but endovascular therapy with metallic stenting may be palliative in some cases.
References: Kapur S, Paik E, Rezaei A, et al. Where there is blood, there is a way: unusual collateral vessels in superior and inferior vena cava obstruction. Radiographics 2010;30(1):67–78.
Sheth S, Ebert MD, Fishman EK. Superior vena cava obstruction evaluation with MDCT. AJR Am J Roentgenol 2010;194(4):W336–W346.
41 Answer C.Malignant portal vein thrombosis (PVT) is a contraindication to liver transplantation by the Milan criteria. Patients with malignant PVT have advanced hepatocellular carcinoma (HCC) and poor prognosis, with a high rate of recurrence after transplant.
Liver transplantation has found to be an effective treatment for some patients with HCC that is unresectable because of tumor location, multifocality, or severe hepatic insufficiency. Transplantation has the potential for correcting liver dysfunction as well as removing the malignancy. Prognosis of HCC was generally poor regardless of treatment. However, patient selection for liver transplantation using the Milan criteria has been associated with positive outcomes, including 4-year overall survival of 85% and recurrence rate of 8%. Patients meeting criteria have a single tumor ≤5 cm or up to three tumors each ≤3 cm. Vascular invasion and extrahepatic metastases are exclusion criteria. The Milan criteria have been adopted by the United Network for Organ Sharing (UNOS) and Medicare to identify patients with HCC to determine eligibility for transplant, although more recently, there has been research into expanding the eligibility criteria to offer transplants to a larger patient population with HCC. Hepatic encephalopathy and refractory variceal bleeding are among the acceptable indications for liver transplant.
References: Bhargava P, Vaidya S, Dick AA, et al. Imaging of orthotopic liver transplantation: review. AJR Am J Roentgenol 2011;196(3 Suppl):WS15–WS25; Quiz S35-38.
Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334(11):693–699.
42 Answer D.The most common cause of graft failure after liver transplant is rejection. Imaging evaluation when a liver transplant complication is suspected usually begins with ultrasound. Elevated resistive indices of >0.8 may be seen on ultrasound in rejection but are nonspecific. The main role of imaging is to identify structural abnormalities that clinically mimic rejection, including hydronephrosis, vascular complications, and biliary complications. CT, MRI, and nuclear medicine hepatobiliary scans may be helpful for subsequent problem solving. Biopsy is required for definitive diagnosis of rejection.
References: Camacho JC, Coursey-Moreno C, Telleria JC, et al. Nonvascular post-liver transplantation complications: from ultrasound screening to cross-sectional and interventional imaging. Radiographics 2015;35(1):87–104.
Norton PT, DeAngelis GA, Ogur T, et al. Noninvasive vascular imaging in abdominal solid organ transplantation. AJR Am J Roentgenol 2013;201(4):W544–W553.
43 Answer B.The most recent scan shows a nodular focus of arterial enhancement at the margin of the ablation cavity where no enhancement was present several months before. Findings are most consistent with recurrent hepatocellular carcinoma. Notice that both arterial images were obtained with appropriate timing in the late arterial phase with a blush of contrast seen in the main portal vein. Scans performed too early or too late may miss hypervascular liver lesions. Imaging after locoregional therapy such as chemoembolization, radiofrequency ablation, and microwave embolization for HCC is performed to assess treatment response and evaluate for new or recurrent malignancy. Studies performed a short interval (<1 month) after ablation can demonstrate ring-like or ill-defined perilesional altered enhancement thought to represent postprocedural injury and inflammation. This enhancement may mimic residual or recurrent neoplasm. These postprocedural changes should improve or resolve as the normal tissue heals around the cavity. New nodular foci that develop afterward would be suspicious for recurrent neoplasm.
References: Park MH, Rhim H, Kim YS, et al. Spectrum of CT findings after radiofrequency ablation of hepatic tumors. Radiographics 2008;28(2):379–390; discussion 390–372.
Sainani NI, Gervais DA, Mueller PR, et al. Imaging after percutaneous radiofrequency ablation of hepatic tumors: Part 2. Abnormal findings. AJR Am J Roentgenol 2013;200(1):194–204.
44 Answer C.This is a pulsatile flow artifact with ghosting projected over the left lobe of the liver on this noncontrast T1W image. The ghost is the same size and shape as the aorta and should not be mistaken for a hepatic lesion. Flow effects due to the entry phenomenon may cause unwanted artifacts from blood entering the slice plane from above (aorta on the superior slices) or from below (IVC on the inferior slices). Pulsatile flow artifacts cause ghosting at constant intervals in the phase-encoding direction. In the presence of flow, phase shifts occur that are not accounted for by the rephasing gradient that usually follows the initial pulse. In the abdomen, phase encoding is usually applied in the shorter anterior–posterior dimension to decrease scan time. As a result, the ghosting from the aorta often maps into the left hepatic lobe.
To manage this artifact, the phase- and frequency-encoding directions can be swapped to project the ghost out of the area of interest. This usually lengthens the scan time. Presaturation pulses (“sat bands”) can be placed above the imaged area to eliminate the signal from the incoming aortic flow (or placed below the imaged area to eliminate the signal from the incoming IVC flow). Techniques to compensate for flow artifacts include gradient moment nulling, which involves the application of additional pulses to correct for phase shifts within moving protons.
Radiofrequency (RF) interference is seen as a band or bands of noise across the image, usually in the frequency direction. The MRI room is constructed with heavy shielding as a “Faraday cage” to prevent interference from unwanted RF signal, but occasionally, a stray RF signal occurs and is picked up by the MRI receive coil. This can happen if the door is left open or inadequately sealed, electronic equipment is brought into the room, or a scanner component is defective. A liver lesion is unlikely to exactly match the aorta in size, shape, and alignment. Regardless, on this T1W image, a simple cyst and a hemangioma should appear hypointense to the surrounding liver.
References: Huang SY, Seethamraju RT, Patel P, et al. Body MR imaging: artifacts, k-space, and solutions. Radiographics 2015;35(5):1439–1460.
Morelli JN, Runge VM, Ai F, et al. An image-based approach to understanding the physics of MR artifacts. Radiographics 2011;31(3):849–866.
45 Answer A.This patient has imaging findings consistent with hepatic artery stenosis (HAS). Spectral Doppler waveform is being recorded in the hepatic artery (white arrow) at the porta hepatis. This is a classic tardus et parvus waveform in the vessel downstream from a stenosis, with delayed arterial upstroke and decreased peak velocity resulting in a low resistive index (RI) of <0.5 (yellow arrow, RI = 0.4). The stenosis is revealed on the selective arteriogram as focal narrowing (black arrow).
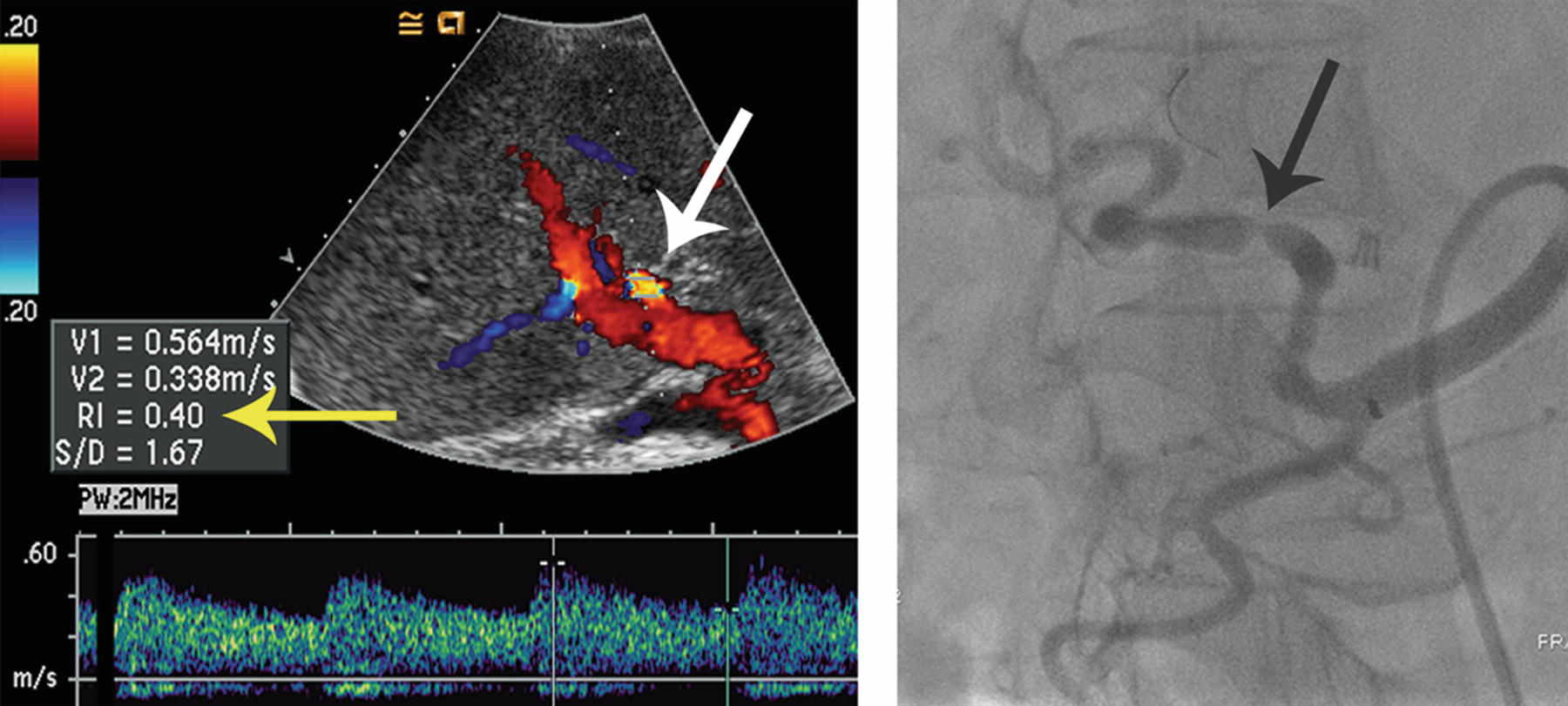
The most common vascular complications following liver transplant involve the hepatic artery. HAS and thrombosis each occur in up to 12% of transplants. HAS occurs most frequently at the anastomosis. Findings typical of HAS besides downstream parvus et tardus waveform on ultrasound include elevated velocity of >200 cm/s and focal aliasing immediately beyond the stenosis. Angiography can be diagnostic and therapeutic.
Because the hepatic artery is the sole source of vascular supply to the bile ducts, arterial compromise can lead to biliary ischemia with formation of bilomas and graft dysfunction. The small hepatic hypodensities (arrows) on the following CT image in the same patient represent developing bilomas.
Developing bilomas in liver transplant patient with HAS.
The other vascular complications (portal vein thrombosis, pseudoaneurysm, and arterioportal fistulas in the answer choices) are possible in liver transplant patients but less common and are not compatible with the imaging findings. The main portal vein is patent on the color Doppler image with appropriate direction of flow (red in this case representing hepatopedal flow toward the liver as indicated by the color reference bar on the left). A pseudoaneurysm is an enlargement, not narrowing, of the artery. An arterioportal shunt would show early venous opacification on arteriogram.
References: Crossin JD, Muradali D, Wilson SR. Ultrasound of liver transplants: normal and abnormal. Radiographics 2003;23(5):1093–1114.
Singh AK, Nachiappan AC, Verma HA, et al. Postoperative imaging in liver transplantation: what radiologists should know. Radiographics 2010;30(2):339–351.
46 Answer A.Giant cavernous hemangiomas (GCAs) can be associated with Kasabach-Merritt syndrome. In this syndrome, thrombocytopenia is caused by sequestration and destruction of platelets within a GCA. The syndrome is usually seen in infants but can also be observed in adults. Size criteria for giant cavernous hemangiomas have been proposed ranging from >4 to >10 cm in size. GCAs usually exhibit the classic peripheral nodular discontinuous enhancement of cavernous hemangiomas as shown in this case. They may have a T2 bright central scar that does not fill in completely on delayed imaging, also demonstrated in this patient. The heterogeneity and atypical appearance of some GCAs occasionally present a diagnostic challenge. GCAs account for fewer than 10% of hemangiomas and uncommonly become symptomatic. Complications include pain, rupture, or Kasabach-Merritt syndrome.
Carcinoid syndrome is flushing and diarrhea that can be seen in some patients with metastatic neuroendocrine tumors. Cushing syndrome is related to hypercortisolism, which can manifest as weight gain, androgen excess, glucose intolerance, and bone loss, among other symptoms. Lambert-Eaton syndrome is a neuromuscular condition manifesting as muscle weakness. It may be seen as a paraneoplastic syndrome associated with small cell lung cancer.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Coumbaras M, Wendum D, Monnier-Cholley L, et al. CT and MR imaging features of pathologically proven atypical giant hemangiomas of the liver. AJR Am J Roentgenol 2002;179(6):1457–1463.
47 Answer C.Multifocal steatosis is seen in a patchy nodular distribution in the liver. The CT shows areas of decreased density. These areas correspond to loss of signal intensity on the out-of-phase images compared to the in-phase image in keeping with microscopic fat. On imaging, steatosis may be diffuse, focal, or multifocal. Classic locations of focal steatosis include areas periportal regions, around the gallbladder fossa, and around the falciform ligament anteriorly. Some cases show striking perivascular distribution as shown in this case and on the following venous phase CT image from a different patient. Multifocal steatosis can mimic metastatic disease or infiltrative malignancy, but there is no underlying parenchymal distortion, displacement of vessels, or other mass effect. Areas of steatosis represent hepatocytes with intracellular lipid and will show enhancement, although they remain hypodense relative to the surrounding liver on the different phases.
Perivascular distribution of hepatic steatosis.
References: Cassidy FH, Yokoo T, Aganovic L, et al. Fatty liver disease: MR imaging techniques for the detection and quantification of liver steatosis. Radiographics 2009;29(1):231–260.
Hamer OW, Aguirre DA, Casola G, et al. Fatty liver: imaging patterns and pitfalls. Radiographics 2006;26(6):1637–1653.
48 Answer B.There is micronodular cirrhosis with numerous regenerative nodules. The representative nodule indicated by the arrow is bright on the arterial phase. Correlation with the precontrast T1 image reveals that the nodule is inherently T1 bright as are the other nodules without convincing arterial enhancement. On the delayed images, there is the nodules become isointense to surrounding liver with no apparent “washout.” Findings are most consistent with regenerative nodules.
T1 hyperintensity within nodules in the setting of cirrhosis has been attributed to steatosis, glycogen, copper, or hemorrhage. In this case, the nodules remain bright on the out-of-phase T1W image with no evidence of microscopic fat and bright on the FS T1W image,with no evidence of macroscopic fat. T1 hyperintense lesions in the diseased liver are not uncommon and often represent regenerative nodules, although on occasion dysplastic nodules or hepatocellular carcinomas show noticeable T1 hyperintensity. Regenerative and dysplastic nodules retain contrast on 20-minute hepatobiliary phase if a hepatobiliary contrast agent is used (not shown). Nodules that are T1 hyperintense may be better evaluated on CT, if they are not bright on precontrast CT images. This makes assessment of enhancement pattern more straightforward.
References: Boland GWL, Halpert RD. Chapter 6: Liver. In: Boland GWL, Halpert RD (eds). Gastrointestinal imaging: the requisites, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2014:218–290.
Hanna RF, Aguirre DA, Kased N, et al. Cirrhosis-associated hepatocellular nodules: correlation of histopathologic and MR imaging features. Radiographics 2008;28(3):747–769.
49 Answer D.This patient has hepatic infarction. The liver on the initial CT is heterogeneous with multiple areas of hypodensity and hypoenhancement, worst in the right lobe. This has a peripheral, geographic appearance without displacement of vessels or mass effect. Note the perisplenic high density consistent with hemoperitoneum as stated in the history. This patient suffered shock as a result of the severe hemorrhage, leading to the infarct. On noncontrast CT a month later, there is a wedge-shaped hypodensity with atrophy and capsular retraction in the right lobe consistent with evolution of the infarct and scarring.
Hepatic infarction is uncommon because the liver has dual blood supply from the hepatic arterial and portal venous systems. Causes for hepatic infarct may include shock, anesthesia, sepsis, trauma, metastases, and percutaneous hepatic interventions such as transarterial chemoembolization and radiofrequency ablation. Hepatic infarct is difficult to diagnose early, and imaging findings may be subtle. Areas of hypoenhancement are typically peripheral and wedge shaped. Margins become sharper and better defined with time. Infiltrative hepatocellular carcinoma (HCC) can also be heterogeneous and ill-defined but tends to show some arterial enhancement and without atrophy. Geographic areas of hypodensity without mass effect resemble areas of steatosis, but findings were acute compared to a recent prior CT, and steatosis does not evolve into a focal scar.
References: Gore RM, Ba-Ssalamah A. Chapter 90: Vascular disorders of the liver and splanchnic circulation. In: Gore RM, Levine MS (eds). Textbook of gastrointestinal radiology, 4th ed. Philadelphia, PA: Elsevier/Saunders, 2015:1676–1705.
Torabi M, Hosseinzadeh K, Federle MP. CT of nonneoplastic hepatic vascular and perfusion disorders. Radiographics 2008;28(7):1967–1982.
50 Answer A.There are multiple small T1 and T2 hypointense nodules in a cirrhotic liver. These lose signal on the in-phase compared to out-of-phase images, most consistent with iron-containing siderotic nodules. There is no arterial enhancement. Although siderotic nodules may be regenerative or dysplastic, they rarely are found to contain malignancy. It is hypothesized that nodules that transition to hepatocellular carcinoma lose the ability to store iron. Patients with cirrhosis and other chronic liver diseases can have abnormally increased iron absorption causing foci of hepatic iron deposition.
References: Baron RL, Peterson MS. From the RSNA refresher courses: screening the cirrhotic liver for hepatocellular carcinoma with CT and MR imaging: opportunities and pitfalls. Radiographics 2001;21:Spec No.: S117-132.
Curvo-Semedo L, Brito JB, Seco MF, et al. The hypointense liver lesion on T2W MR images and what it means. Radiographics 2010;30(1):e38.
51 Answer D.Areas of bright signal intensity are seen on this fat-saturated T2W spin-echo image in the perihepatic fat anterior to the liver as well as within the subcutaneous fat peripherally (arrows). These represent areas of poor fat saturation as the result of field inhomogeneity. Poor fat saturation should not be mistaken for pathology such as ascites or fatty infiltration. A clue to uneven fat saturation artifact is location in areas prone to magnetic field inhomogeneity and susceptibility artifacts, such at the image periphery, at interfaces with the lung, or near metallic objects. Among the choices, moiré fringes are artifacts that also occur in the periphery but have a distinctive appearance of banding not seen in this case.
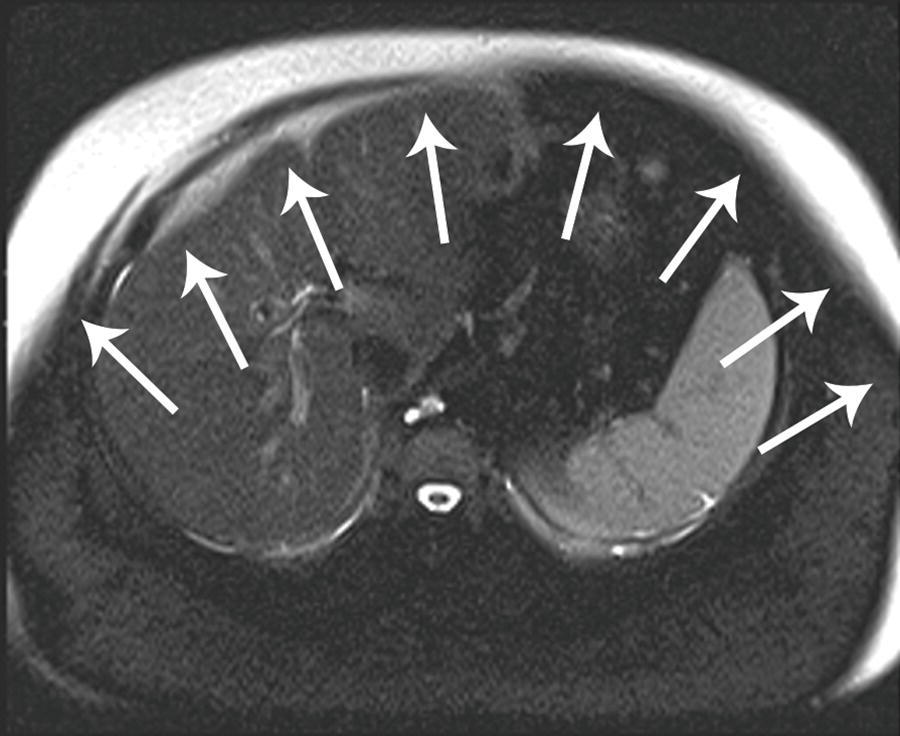
The effectiveness of frequency-selective fat saturation depends on the uniformity of the magnetic field. Factors that cause field inhomogeneity will unpredictably shift the frequency of the fat peak, preventing the fat peak from being identified and crushed (saturated) by the spoiler gradient. To improve fat saturation and generally decrease the effects of susceptibility:
- Move the anatomy of interest toward the isocenter, where the magnetic field is more homogeneous.
- Perform shimming, which adjusts the radiofrequency transmission elements to improve homogeneity of the magnetic field.
- Apply sequences that are less affected by susceptibility artifacts.
- A short tau inversion recovery (STIR) sequence achieves fat suppression without relying on frequency selection of the fat peak and would produce better results at the expense of signal to noise ratio.
- Spin-echo sequences and sequences with shorter TE are less affected by susceptibility than gradient-echo and longer TE sequences.
- A short tau inversion recovery (STIR) sequence achieves fat suppression without relying on frequency selection of the fat peak and would produce better results at the expense of signal to noise ratio.
References: Huang SY, Seethamraju RT, Patel P, et al. Body MR imaging: artifacts, k-space, and solutions. Radiographics 2015:140289.
Morelli JN, Runge VM, Ai F, et al. An image-based approach to understanding the physics of MR artifacts. Radiographics 2011;31(3):849–866.
52 Answer C.A prominent arterioportal shunt (fistula) is identified in the cirrhotic liver. Spectral Doppler image is labeled “MPV” and demonstrates hepatofugal flow with reversal of flow in the main portal vein. There is arterialization of portal vein waveform with regular pulsatility, not respiratory variation. Arterial phase CT images demonstrate a serpiginous blush of contrast in the hepatic dome. There is early intense opacification of the right portal vein (arrowhead), following the attenuation of the adjacent right hepatic artery (arrow).
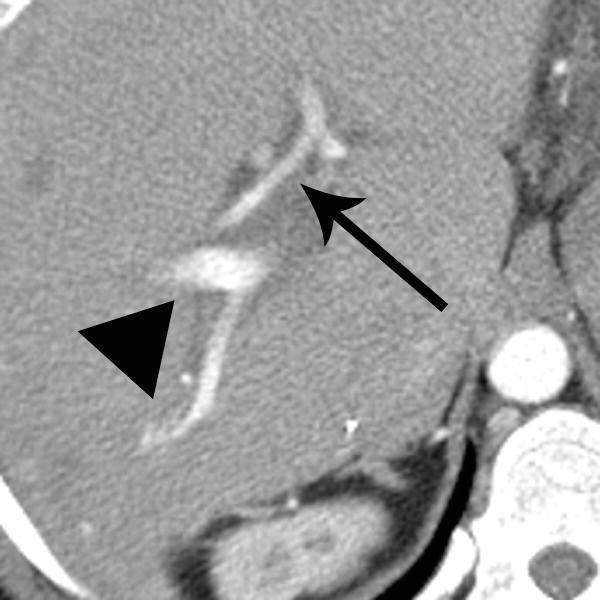
Other findings that may be seen in arterioportal shunt/fistula include enlargement of the feeding artery with low-resistance waveform. The portal vein may be dilated. Color Doppler “speckling” may be identified within the liver parenchyma adjacent to the fistula, an artifact manifesting as a small cluster of various colors due to tissue vibration. Perfusion abnormalities may be seen, with focal or wedge-shaped transient hepatic attenuation differences (THADs) on CT and transient hepatic intensity differences (THIDs) on MRI. Small shunts may mimic small hypervascular masses such as hepatocellular carcinoma, focal nodular hyperplasia, and hemangiomas. Large intrahepatic shunts can cause severe portal hypertension and heart failure. Arteriogram can be diagnostic and therapeutic. Acquired causes include cirrhosis, neoplasms (particularly hepatocellular carcinoma), trauma, biopsy, and surgery. Congenital arterioportal fistulas may be idiopathic or associated with hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu syndrome), Ehlers-Danlos syndrome, and biliary atresia.
References: Gallego C, Miralles M, Marín C, et al. Congenital hepatic shunts. Radiographics 2004;24(3):755–772.
Torabi M, Hosseinzadeh K, Federle MP. CT of nonneoplastic hepatic vascular and perfusion disorders. Radiographics 2008;28(7):1967–1982.
53a Answer B.This lesion has a centrifugal enhancement pattern, which has been described as the most common enhancement pattern associated with peliosis hepatis (from the Greek pelios meaning “dusky” or “purple”). Peliosis hepatis is a rare benign vascular disorder characterized by dilated sinusoids and blood-filled cavities lined by endothelium. On arterial phase in this case, there is central globular enhancement which progresses outward toward the periphery and remains hyperdense to surrounding liver on the delayed phase. This centrifugal inner-to-outer pattern is the opposite of the centripetal outer-to-inner pattern of fill-in seen with hemangiomas. On late phases, peliosis may show persistent enhancement indicating blood pooling as in this case or isointensity to surrounding liver. Centrifugal enhancement is the classic pattern in peliosis hepatis although peliosis may exhibit other patterns of enhancement. Note that a centrifugal enhancement pattern is not specific for peliosis and may occasionally be seen with metastases. However, in this case, the persistent enhancement greater than liver on delayed phases favors peliosis over hypervascular metastases. Lymphoma secondarily involving the liver is more common than primary hepatic lymphoma and is an incorrect answer choice because it is hypoenhancing. Cholangiocarcinoma (not an answer choice) can show delayed enhancement, but the mass is typically shows little arterial enhancement and may be associated with biliary ductal dilation.
Peliosis hepatis tends to have little mass effect on adjacent vessels compared to hemangiomas and other tumors. This is demonstrated below on the CT of a different patient with multiple hypoenhancing foci of peliosis hepatis. A branch of the right hepatic vein (black arrow) passes along side the margin of the dominant lesion undisturbed. Involvement may be diffuse or focal, with lesions of variable size. Lesions may have variable internal density from blood products (white arrow). Peliosis may involve other organs such as the spleen, lymph nodes, lungs, and skin.
Peliosis hepatis.
References: Iannaccone R, Federle MP, Brancatelli G, et al. Peliosis hepatis: spectrum of imaging findings. AJR Am J Roentgenol 2006;187(1):W43–W52.
Torabi M, Hosseinzadeh K, Federle MP. CT of nonneoplastic hepatic vascular and perfusion disorders. Radiographics 2008;28(7):1967–1982.
53b Answer A.The pathogenesis of peliosis hepatis is unclear although drugs, toxins, and infections have been implicated. Up to half of cases are idiopathic. Bartonella henselae and Bartonella quintana are the bacteria responsible for a type of peliosis called bacillary peliosis that is seen in AIDS patients. Most patients are asymptomatic and diagnosed incidentally, although there are reports of rupture and progression to cirrhosis and portal hypertension. Additional imaging modalities, follow-up imaging, and biopsy may factor into patient management because lesions may be mistaken for metastases or other primary hepatic tumors. Lymphadenopathy may be prominent in bacillary peliosis caused by B. henselae. Lesions can regress after treatment of the underlying cause. Bacillary peliosis caused by Bartonella infections is treated with antibiotics.
References: Savastano S, San Bortolo O, Velo E, et al. Pseudotumoral appearance of peliosis hepatis. AJR Am J Roentgenol 2005;185(2):558–559.
Torabi M, Hosseinzadeh K, Federle MP. CT of nonneoplastic hepatic vascular and perfusion disorders. Radiographics 2008;28(7):1967–1982.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree